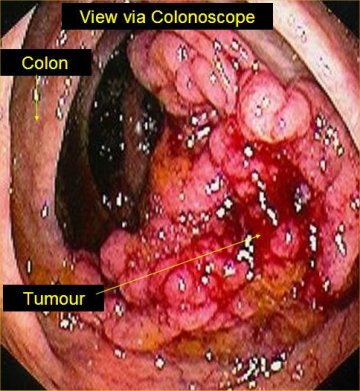
 Definition of colon cancer: Cancer that forms in the tissues of the colon (the longest part of the large intestine). Most colon cancers are adenocarcinomas (cancers that begin in cells that make and release mucus and other fluids).
Definition of colon cancer: Cancer that forms in the tissues of the colon (the longest part of the large intestine). Most colon cancers are adenocarcinomas (cancers that begin in cells that make and release mucus and other fluids).Surgery is the most common treatment for colorectal cancer. During surgery, the tumor, a small margin of the surrounding healthy bowel, and adjacent lymph nodes are removed. The surgeon then reconnects the healthy sections of the bowel. In patients with rectal cancer, the rectum is permanently removed. The surgeon then creates an opening (colostomy) on the abdomen wall through which solid waste in the colon is excreted.
Specially trained nurses (enterostomal therapists) can help patients adjust to colostomies, and most patients with colostomies return to a normal lifestyle.
The long-term prognosis after surgery depends on whether the cancer has spread to other organs (metastasis). The risk of metastasis is proportional to the depth of penetration of the cancer into the bowel wall. In patients with early colon cancer which is limited to the superficial layer of the bowel wall, surgery is often the only treatment needed. These patients can experience long-term survival in excess of 80%. In patients with advanced colon cancer, wherein the tumor has penetrated beyond the bowel wall and there is evidence of metastasis to distant organs, the five-year survival rate is less than 10%.
In some patients, there is no evidence of distant metastasis at the time of surgery, but the cancer has penetrated deeply into the colon wall or reached adjacent lymph nodes. These patients are at risk of tumor recurrence either locally or in distant organs. Chemotherapy in these patients may delay tumor recurrence and improve survival.
Chemotherapy is the use of medications to kill cancer cells. It is a systemic therapy, meaning that the medication travels throughout the body to destroy cancer cells. After colon cancer surgery, some patients may harbor microscopic metastasis (small foci of cancer cells that cannot be detected). Chemotherapy is given shortly after surgery to destroy these microscopic cells. Chemotherapy given in this manner is called adjuvant chemotherapy. Recent studies have shown increased survival and delay of tumor recurrence in some patients treated with adjuvant chemotherapy within five weeks of surgery. Most drug regimens have included the use of 5-flourauracil (5-FU). On the other hand, chemotherapy for shrinking or controlling the growth of metastatic tumors has been disappointing. Improvement in the overall survival for patients with widespread metastasis has not been convincingly demonstrated.
Chemotherapy is usually given in a doctor's office, in the hospital as a outpatient, or at home. Chemotherapy is usually given in cycles of treatment periods followed by recovery periods. Side effects of chemotherapy vary from person to person, and also depend on the agents given. Modern chemotherapy agents are usually well tolerated, and side effects are manageable. In general, anticancer medications destroy cells that are rapidly growing and dividing. Therefore, red blood cells, platelets, and white blood cells are frequently affected by chemotherapy. Common side effects include anemia, loss of energy, easy bruising, and a low resistance to infections. Cells in the hair roots and intestines also divide rapidly. Therefore, chemotherapy can cause hair loss, mouth sores, nausea, vomiting, and diarrhea.
Radiation therapy in colorectal cancer has been limited to treating cancer of the rectum. There is a decreased local recurrence of rectal cancer in patients receiving radiation either prior to or after surgery. Without radiation, the risk of rectal cancer recurrence is close to 50%. With radiation, the risk is lowered to approximately 7%. Side effects of radiation treatment include fatigue, temporary or permanent pelvic hair loss, and skin irritation in the treated areas.
Other treatments have included the use of localized infusion of chemotherapeutic agents into the liver, the most common site of metastasis. This involves the insertion of a pump into the blood supply of the liver which can deliver high doses of medicine directly to the liver tumor. Response rates for these treatments have been reported to be as high as eighty percent. Side effects, however, can be serious. Additional experimental agents considered for the treatment of colon cancer include the use of cancer-seeking antibodies bound to cancer-fighting drugs. Such combinations can specifically seek and destroy tumor tissues in the body. Other treatments attempt to boost the immune system, the bodies' own defense system, in an effort to more effectively attack and control colon cancer. In patients who are poor surgical risks, but who have large tumors which are causing obstruction or bleeding, laser treatment can be used to destroy cancerous tissue and relieve associated symptoms. Still other experimental agents include the use of photodynamic therapy. In this treatment, a light sensitive agent is taken up by the tumor which can then be activated to cause tumor destruction.
|
Bookmark this post:
|
|

0 comments
Post a Comment