 What is brucellosis?
What is brucellosis? Brucellosis is an infectious disease caused by bacteria from the genus Brucella. It is an infection that affects mainly animals, including goats, sheep, camels, pigs, elk, deer, cattle, and dogs. Humans develop brucellosis when they come in contact with contaminated animals or animal products. The symptoms of brucellosis often resemble a flu-like illness.
Human brucellosis is a disease that is found worldwide, and it has an annual occurrence rate of more than 500,000 cases. Brucellosis tends to occur more commonly in regions with less established animal-disease-control programs and in areas where public-health initiatives may be less effective. High-risk areas include the Mediterranean Basin (Portugal, Spain, Southern France, Italy, Greece, Turkey, and North Africa), South and Central America, Eastern Europe, Africa, Asia, the Caribbean, and the Middle East. In the United States, brucellosis is much less common, with only 100-200 human cases reported each year. This decrease in cases in the United States is felt to be due to effective animal vaccination programs and milk pasteurization.
What is the history of brucellosis?
Brucellosis is a disease that is thought to have existed since ancient times, as it was first described more than 2,000 years ago by the Romans and Hippocrates. It was not until 1887 that a British physician, Dr .David Bruce, isolated the organism that causes brucellosis from several deceased patients from the island of Malta. This disease has had several names throughout its history, including Mediterranean fever, Malta fever, Crimean fever, Bang's disease, and undulant fever (because of the relapsing nature of the fever associated with the disease).
In the mid-20th century, the Brucella bacteria was also developed for use as a biological weapon by the United States. The use of brucellosis for biological warfare purposes was later banned in 1969 by President Nixon.
What causes brucellosis?
Brucellosis is a systemic infectious disease transmitted from certain animals to humans (zoonotic disease). Brucellosis in humans is predominantly caused by four different species of Brucella bacteria: Brucella melitensis (goats, sheep, camels), Brucella suis (pigs), Brucella abortus (cows, buffalo, elk, camels, yaks), and Brucella canis (dogs). Though all of these species can cause human brucellosis, Brucella melitensis is the most prevalent worldwide, and it is felt to cause the most severe cases of brucellosis.
How is brucellosis transmitted?
Brucellosis is transmitted from animals to humans in several ways. The most common route of transmission occurs when humans consume raw milk or cheese from infected sheep and goats. Infected animals shed the organism into their milk, and if humans eat or drink unpasteurized dairy products from these affected animals, they can develop brucellosis.
Brucellosis can also be transmitted to humans via inhalation of the organism or by direct contact with infected animal secretions. The bacteria can gain entry into the body through the inhalation of aerosolized secretions, through breaks in the skin, or through exposure of the mucous membranes/conjunctiva from the splashing of infected secretions. With these routes of entry, brucellosis is an occupational disease that can affect veterinarians, slaughterhouse workers, butchers, hunters, laboratory personnel, and those individuals who work closely with livestock (for example, farmers and shepherds).
Finally, an accidental injection with the livestock vaccine used against Brucella abortus can also lead to brucellosis in humans. Human-to-human transmission is very rare (via sexual contact and breastfeeding).
What are the symptoms and signs of brucellosis?
The symptoms and signs of brucellosis may develop from days to months after the initial exposure to the organism (incubation period). While some individuals may develop mild symptoms, others may go on to develop long-term chronic symptoms.
The signs and symptoms of brucellosis are extensive and they can be similar to many other febrile illnesses. They include
- fever (the most common finding, and it may be intermittent and relapsing),
- sweating,
- body aches,
- joint pain,
- fatigue,
- weakness,
- dizziness,
- headache,
- depression,
- irritability,
- loss of appetite,
- weight loss,
- cough,
- difficulty breathing,
- chest pain,
- abdominal pain,
- enlarged liver and/or spleen.
Other symptoms and signs may also be present with brucellosis. Certain variables such as the severity of illness, the chronicity of illness, and the development of complications can all impact the clinical findings associated with the disease.
How is brucellosis diagnosed?
Making the diagnosis of brucellosis can sometimes be difficult because of the similar symptoms and signs shared with other febrile illnesses. An accurate history obtained by your health-care provider (including travel history, occupation, animal exposure, etc.) may be very helpful in raising the suspicion of brucellosis as a possible diagnosis.
In general, blood tests and blood/tissue cultures are necessary for making the diagnosis of brucellosis. Common blood tests used to make the diagnosis include testing for antibodies against the bacteria and isolating the organism from blood cultures. A biopsy of body tissue (from the bone marrow or the liver, for example) can also assist in making the diagnosis. Additional blood tests may demonstrate anemia, low platelets, a low white blood cell count, and elevated liver function tests.
Other imaging studies and procedures may also be performed initially depending on the individual's signs and symptoms. These tests may include CT scan, MRI, X-ray, ultrasound, lumbar puncture (spinal tap), joint aspiration, or an electrocardiogram (ECG).
What is the treatment for brucellosis?
The cornerstone of treatment for brucellosis is antibiotics. Because of the high relapse rate associated with the disease, the use of a multidrug (two or more) antibiotic regimen is recommended. The antimicrobials most commonly used include doxycycline (Vibramycin), streptomycin, rifampin (Rifadin), gentamicin (Garamycin), and trimethoprim-sulfamethoxazole (Bactrim, Septra). The combination of antibiotics used will vary based on disease severity, age and pregnancy.
In general, a full six-week course of antibiotics is recommended, and prompt treatment can lead to an improvement in symptoms and may also prevent the complications associated with brucellosis. However, relapse rates of the disease are still about 5%-10%, even with treatment. Depending on the severity of illness, the associated complications (if any) and the timing of treatment, recovery may take from a few weeks to a few months.
Rarely, surgical intervention may be needed for certain complications associated with brucellosis, such as abscess formation or heart-valve infection. Your health-care provider may need to consult other physicians, including surgeons, infectious disease specialists, or a neurologist.
What are the complications of brucellosis?
In general, if treated appropriately with antibiotics in a timely manner after the onset of symptoms, the prognosis for patients with brucellosis is excellent. The mortality rate is low (<2%).>
- Bones and joints
- Sacroiliitis, spondylitis, and osteomyelitis
- Cardiovascular
- Endocarditis (a primary cause of death), myocarditis, and pericarditis
- Central nervous system (neurobrucellosis)
- Meningoencephalitis
- Gastrointestinal
- Hepatitis, hepatic abscess, colitis, and spontaneous peritonitis
- Genitourinary
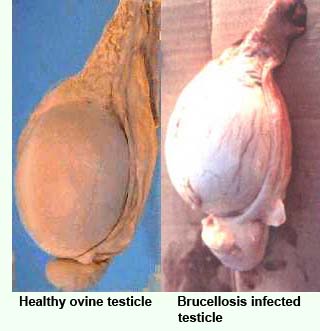
- Orchitis
- Pulmonary
- Pneumonia
- Ocular
- Optic neuritis and uveitis
How can brucellosis be prevented?
The prevention of brucellosis can be achieved through various measures. The most important step in preventing brucellosis in humans begins with the control and/or eradication of the infection in animals who serve as a reservoir. This requires a coordinated effort between local public-health organizations and animal-disease-control entities. The most effective measures to achieve this objective include animal vaccination programs, animal testing, and the elimination of infected animals. There is no human vaccine currently available.
In areas where eradication of the disease may not be possible, preventive measures are aimed at reducing the risk of transmission to humans. These measures may include
- pasteurization of dairy products;
- avoiding the consumption of unpasteurized dairy products, including milk and cheese;
- avoiding the consumption of undercooked meat;
- using appropriate barrier precautions (goggles, gloves, masks, etc) to avoid exposure to aerosols and body fluids for those with an occupational risk for brucellosis;
- warning laboratory workers about potentially infected specimens so that appropriate biosafety level III precautions can be taken.
Brucellosis At A Glance
- Brucellosis is an infectious disease caused by bacteria from the genus Brucella.
- Brucellosis is an infection of certain animals that is transmitted to humans.
- Humans acquire brucellosis when they come in contact with contaminated animals or animal products, most commonly from the ingestion of raw milk or cheese.
- The symptoms of brucellosis may include fever, sweating, body aches, and joint pain.
- Brucellosis is typically diagnosed through blood tests and by isolating the organism from blood and other body tissues.
- A multidrug antibiotic regimen is the cornerstone of treatment for brucellosis.
- The complications of brucellosis may involve various organ systems.
- Brucellosis can be prevented by animal-disease-control measures, avoidance of unpasteurized dairy products, and occupational protective measures.
REFERENCES:
Al Nassir, Wafa, Michelle V. Lisgaris, Robert A. Salata. "Brucellosis." eMedicine. Feb. 3, 2009.
Maloney Jr., Gerald E. "CBRNE-Brucellosis." eMedicine. Apr. 29, 2009.
Switzerland. "Brucellosis (Human)." World Health Organization.
Switzerland. "Brucellosis." World Health Organization.
United States. "Brucellosis." Centers for Disease Control and Prevention. Dec. 7, 2007.
|
Bookmark this post:
|
|

0 comments
Post a Comment