
How does the heart work?
The heart is a two stage electric pump whose job it is to circulate blood through the body. The pump is dependent on the electric current that the cells of the heart generate to have a coordinated squeeze so that the pump can pump.
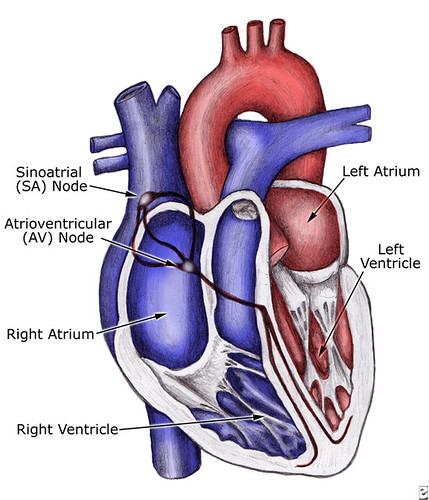
The heart has four chambers, the right and left atria (singular= atrium) and the right and left ventricles. The right side of the heart pumps blood to the lungs while the left side pumps it to the rest of the body.
Blood from the body is collected in the right atrium and is pushed into the right ventricle with a small beat of the upper chamber of the heart. The right ventricle pumps the blood to the lungs to pick up oxygen, and the oxygenated blood from the lungs returns to the left atrium, where the small atrial beat pushes it to the left ventricle. The left ventricle is much thicker than the right because it needs to be strong enough to send blood to the entire body.
There are special cells in the right atrium called the sino-atrial node (SA node) that generate the first electrical impulse, allowing the heart to beat in a coordinated way. The SA node is considered the "natural pacemaker" of the heart. This pacemaker function begins the electrical impulse which follows pathways in the atrial walls, almost like wiring, to a junction box between the atrium and ventricle called the atrio-ventricular node (AV node). This electric signal causes muscle cells in both atria to contract all at once. At the AV node, the electric signal waits for a very short time, usually one to two tenths of a second, to allow blood to leave the atria and fill up the ventricles. The signal then passes through electric bundles in the ventricle walls to allow these chambers to contract, again in a coordinated way, and pump blood to the body.
The SA node generates an electric beat about 60-80 times a minute, and each should result in a heart beat. That beat can be felt as an external pulse. After a heart beat, the muscle cells of the heart need a split second to get ready to beat again, and the electrical system allows a pause for this to happen.

The heart and its electrical activity depend upon a relatively narrow normal state for it to work. Fortunately, the body tends to protect the heart as best as it can. Still, rhythm disturbances are frequent. Some disturbances are normal physiologic responses, but some are potentially life threatening.
Every cell in the heart can act as a pacemaker. The SA node has an intrinsic heart beat generation rate of 60-80. The AV node has a rate of about 40, and the ventricles themselves can generate beats at a rate of about 20 and may kick in if the cells of the upper chamber fail or if the electrical signals to the ventricle are blocked.
Premature atrial contractions (PACs) and premature ventricular contractions (PVCs)
Every person experiences the occasional palpitation, where the atrium or the ventricle beats early. These PACs (premature atrial contractions) or PVCs (premature ventricular contractions) are normal variations and most people are unaware of their occurrence, however, some patients report palpitations in the chest and neck. PACs and PVCs in healthy individuals generally do not pose any health risks.
Sinus tachycardia
The heart, its cells, and its electricity may come under many outside influences where it may beat more quickly. Sinus tachycardia - (sinus=from the SA node + tachy=rapid + cardia + heart) or a rapid regular heartbeat - is a common rhythm issue. It occurs when the body asks the heart to pump more blood, or when the electrical system is stimulated by chemicals.
The body needs increased cardiac output in time of physiologic stress. Cardiac output is the amount of blood the heart pumps in the course of one minute. It can be calculated by the amount of blood that the heart pumps with each beat (stroke volume) multiplied by the heart rate. Since the stroke volume tends not to change too much, it is the heart rate that has to increase to meet the body's needs. Examples include exercise, in which the muscles have greater oxygen requirements and the heart rate speeds up to pump more blood to meet that need, dehydration, in which the stroke volume may fall a little since there is less fluid in the body and the heart rate has to speed up to compensate, or with acute blood loss such as after an accident.
The electrical system can be stimulated in a variety of ways to make the heart beat faster. In times of stress, the body generates adrenaline, and among other symptoms it produces, it can make the heart beat faster. Think of being frightened and feeling your heart race. Increased thyroid hormone levels in the body can also cause a tachycardia. Ingestion of a variety of drugs can also cause the heart to race, including caffeine, alcohol, and over-the-counter cold medications that include drugs like phenylephrine. These compounds get metabolized by the body to act like adrenaline on the heart. Illegal drugs like methamphetamine and cocaine can also cause a sinus tachycardia.Sinus bradycardia
The heart, its cells and its electricity may come under the many outside influences where it may beat more slowly. Sinus bradycardia (brady=slow + cardia=heart) by definition, is a heart beat generated by the SA node at a rate slower than 60 beats per minute. This may be normal in people who are active and athletic or in patients taking medications designed to slow the heart like beta blockers or calcium channel blockers.
Vasovagal syncope is an episode of profound sinus bradycardia associated with a noxious stimulus in which the vagal system of the body kicks in. While the sympathetic system of the body is mediated by adrenaline, the parasympathetic system is mediated by the vagus nerve and the chemical acetylcholine, which promotes the exact opposite body reaction than does adrenaline. In some people, exposure to pain or a difficult emotional situation can stimulate the vagus nerve, slow the heart, and dilate blood vessels (veins), causing cardiac output to decrease and making a person feel lightheaded or faint. It can also happen when one bears down to urinate or have a bowel movement.
Abnormal rhythms
Rhythm disturbances are classified according to whether they arise from the atrium or ventricle, are fast or slow, or regular or irregular.
Tachycardia
Rapid heart rates can originate from either the atrium or the ventricle, but rhythms from the ventricle are more often considered life threatening. The initial approach to rapid heart rates is to quickly identify the rhythm, and if blood pressure is maintained and there is no evidence of a failing heart, then treatment is directed to rate control with the eventual return of the heart back to normal sinus rhythm. If, however, there is evidence that the heart is failing because of the rapid rate, then emergency measures, including using electricity to shock the heart back into a regular rhythm, may be necessary.
Ventricular Fibrillation (V Fib)
Ventricular Fibrillation is technically not a rapid heart rhythm because the heart has ceased to beat. In ventricular fibrillation, the ventricles do not have a coordinated electrical pattern and the ventricles, instead of beating, just jiggle. Since the heart doesn't beat, the body dies. This rhythm is often associated with a heart attack in which the ventricular muscle doesn't get enough blood supply (myocardial ischemia), becomes irritated, and causes the whole ventricle to stop beating. The only treatment for this is defibrillation with an electrical shock. Automated External Defibrillators (AEDs) in public places have helped decrease the mortality from sudden cardiac death, but prevention remains the mainstay to survive this event. Some people, such as those with a very weak heart muscle or who have a prior history of ventricular fibrillation will require an implantable defibrillator to prevent future episodes of sudden death and treat this rhythm. Aside from myocardial ischemia, other causes of ventricular fibrillation may include severe weakness of the heart muscle, electrolyte disturbances, drug overdose, and poisoning.
Ventricular Flutter
Ventricular Flutter is another rapid heart rate that originates in the ventricle. The causes are the same as ventricular fibrillation, but because of the electrical conduction pattern in the heart pathways, an organized signal is provided to the ventricles, allowing them to beat. This remains an emergency, because without treatment, this rhythm will degenerate to ventricular fibrillation.
Paroxysmal supraventricular tachycardia (PSVT)
Paroxysmal supraventricular tachycardia (PSVT) occurs when the pathways in the AV node or atrium allow an altered conduction of electricity, and the atrium begins firing in a regular - fast rate, sometimes more than 150 -200 times per minute. The ventricle, sensing the electrical activity coming through the AV node, beats along with each stimulation, and this tachycardia occurs.
This is rarely a life threatening event, but most people feel uncomfortable when PSVT occurs. They may become lightheaded, weak, have shortness of breath, and describe a feeling of fullness in the throat. PSVT is usually tolerated and can even stop on its own. If this is a first time event, activating EMS (emergency medical services) and calling 911 is important, since other tachycardias can be life threatening.
The treatment for PSVT are attempts at stimulating the vagus nerve to slow the heart (see vasovagal syncope above) by holding one's breath and bearing down as if to have a bowel movement. Intravenous medications are often used to break the episode. Many patients have PSVT due to congenital abnormalities in the conduction system. External causes can include hyperthyroidism, electrolyte imbalances, and the use of caffeine, alcohol, over-the-counter cold medications containing stimulants, or illegal drugs like cocaine and methamphetamine.

Wolfe-Parkinson-White Syndrome
Wolfe-Parkinson-White syndrome is a specific type of PSVT, in which an inborn error of wiring has occurred near the AV node, and an accessory electrical pathway exists. The diagnosis is made by electrocardiogram (EKG), and the treatment may include medications or catheter mediated ablation of the involved pathway.
Atrial Fibrillation (A Fib)
Atrial fibrillation occurs when the atrium has lost the ability to beat in a coordinated fashion. Instead of the SA node generating a single electrical signal, numerous areas of the atrium become irritated and produce electrical impulses. This causes the atrium to jiggle like a bowl of Jell-O instead of beating. The AV node sees all the electrical signals, but because there are so many, and because they are so erratic, only some of the hundreds of signals per minute are passed through to the ventricle. The ventricles then fire irregularly and often very quickly.
As in PSVT, the symptoms may be palpitations, lightheadedness, and shortness of breath. The cause of atrial fibrillation, however, may be more significant, since it may be due to aging of the conducting system of the heart and there may be associated atherosclerotic heart disease. Therefore, atrial fibrillation with rapid ventricular response associated with chest pain or evidence of pulmonary edema (pulmonary=lung +edema=fluid) may need emergent cardioversion (a procedure that uses electricity to shock the heart back into a normal rhythm) or shock therapy.
The long term significant complication of atrial fibrillation is the formation of blood clots along the inside of the heart wall. These clots may break off and travel to different organs in the body blocking blood vessels, and causing the affected organs to malfunction because of the loss of blood supply. A common complication is a clot traveling to the brain, resulting in a stroke.
If the patient presents for medical care within less than 24 hours, then attempts will be made to return the heart to normal sinus rhythm. If this window has passed, there is great risk that during conversion back to a regular rhythm, a blood clot will break loose. Therefore, the strategy to treat atrial fibrillation is time-dependent. Within the first 24 hours, attempts will be made to slow the heart and return it to normal rhythm using medications or electric shock. After this window has passed, the treatment will be focused on rate control only, and anti-coagulation therapy will be offered to prevent blood clot formation.
Aside form the clot issue, atrial fibrillation is a safe rhythm and not life threatening as long as the rate is controlled. Medications are used to slow the electrical impulses through the AV node, so that the ventricles do not try to capture each signal being produced. The reason to return people to a regular rhythm has to do with cardiac output. In atrial fibrillation, the atrium does not beat and pump blood to the ventricle. Instead blood flows into the ventricle by gravity alone. This lack of atrial kick can decrease the heart's efficiency and cardiac output by 10%-15 %.
Anticoagulation with warfarin (Coumadin) is almost always recommended for those patients with atrial fibrillation.
If atrial fibrillation is poorly tolerated due to symptomatic palpitations or symptoms of reduced cardiac output, or if there are concerns with lifelong Coumadin therapy, more definitive therapy may include specific medications, electrical cardioversion, or catheter based ablation (sometimes with an adjunctive pacemaker inserted). Atrial fibrillation is a common condition, with many implications, and the best plan for each patient should be discussed at length with one's physician.
Atrial flutter
Atrial flutter is similar to atrial fibrillation except that instead of having chaotic electrical firing from all points in the atrium, one point has become irritated and can fire 300 times per minute or more. The issues that exist for atrial fibrillation apply to atrial flutter. Atrial flutter may degenerate into atrial fibrillation.
Bradycardia
Aside from medications that are meant to slow the heart for treatment of a variety of medical problems, bradycardia (brady=slow + cardia=heart) is usually due to heart block and the aging of the electrical wiring of the heart. This is no different than the aging of your home's electrical system, but instead of being able to rewire the heart; these conditions may need to be treated with an implantable pacemaker.
Heart blocks
Heart blocks involving the ventricle may be asymptomatic and of little consequence except to point to underlying heart or lung disease. They are diagnosed by EKG.
Heart blocks involving the atrium can be classified as first, second, and third degree.
- First degree heart block is common and of little significance. There is a slight delay in getting the electrical signal from the SA node to the AV node, but the heart functions normally.
- There are two types of second degree heart block (Mobitz I and Mobitz II) but only the Mobitz II type can be a precursor to a life threatening rhythm problem.
- Third degree heart block describes the complete loss of connection between the electrical activity of the atrium and the ventricle. Second and third degree heart blocks are diagnosed by analyzing heart rhythm strips and EKGs.
Heart blocks are symptomatic because the heart beats so slowly that cardiac output is decreased. The symptoms may include lightheadedness or passing out (syncope), weakness, shortness of breath, and chest pain.
Diagnosis and treatment of life-threatening heart block happen at the same time. Often a temporary pacemaker may be placed to stabilize the patient, and then decisions are made as to what type of permanent solution is appropriate.
When to seek medical care
Unexplained palpitations are not normal, especially when associated with shortness of breath, sweating, feelings of chest pressure, or passing out. The person should be laid flat, and EMS (emergency medical service) should be activated by calling 911 or the emergency number in your area. If the person is unconscious, life support should be undertaken following the American Heart Association guidelines.
If the episode is short lived and resolves spontaneously, the primary care provider should be contacted urgently to seek advice.
If the episode is a recurrent problem, the diagnosis is known, and the rhythm disturbance resolves itself, then a less urgent call to the primary care provider is warranted.
One should not be faulted for seeking emergent medical care any time a heart rhythm disturbance occurs.
How are heart rhythm disorders diagnosed?
The mainstay of diagnosis remains the EKG and heart rhythm monitoring. These are often done immediately in the ambulance or upon arrival in the emergency department. Unfortunately, in many patients, the palpitations or symptoms have resolved, and no acute rhythm abnormalities can be found.
Depending on the associated symptoms and the history, observation and monitoring of the heart may occur in hospital or as an outpatient. In patients who are syncopal, meaning that they passed out, and it cannot be explained by a benign diagnosis like vasovagal syncope, admission to the hospital often occurs. Those patients with chest pain and shortness of breath may also be admitted to evaluate their heart; otherwise, monitoring devices that can measure heart rates and rhythms for 24 or 48 hours or longer (up to one month or more) are used. In some instances, rhythm identification is elusive and may take months or years to capture and identify.
If the rhythm is known, then tests to identify potential causes may be done. These are dependent on the specific rhythm abnormality and can range from blood tests to lung evaluations to echocardiograms and electrophysiologic testing.
What is the treatment for heart rhythm disorders?
Treatment is individualized and based upon the diagnosis.
Can heart rhythms be prevented?
Minimizing risk factors for heart disease will be helpful, including controlling blood pressure, lowering cholesterol, keeping diabetes under control, and not smoking.
For those with rapid palpitations that are intermittent, avoiding stimulants like alcohol, caffeine, over-the-counter cold medications, and illicit drugs are important preventive measures.
Source|
Bookmark this post:
|
|


0 comments
Post a Comment