
What is attention deficit hyperactivity disorder (ADHD)?
ADHD refers to a chronic biobehavioral disorder that initially manifests in childhood and is characterized by hyperactivity, impulsivity, and/or inattention. Not all of those affected by ADHD manifest all three behavioral categories. These symptoms can lead to difficulty in academic, emotional, and social functioning. The diagnosis is established by satisfying specific criteria and may be associated with other neurological, significant behavioral, and/or developmental/learning disabilities. Therapy may consider the use of medication, behavioral therapy, and adjustments in day-to-day lifestyle activities.
Studies in the United States indicates approximately 8%-10% of children satisfy diagnostic criteria for ADHD. ADHD is, therefore, one of the most common disorders of childhood. ADHD occurs two to four times more commonly in boys than girls (male to female ratio 4:1 for the predominantly hyperactive type vs. 2:1 for the predominantly inattentive type). Three subtypes of ADHD are described: (1) predominantly inattentive, (2) predominantly hyperactive and impulsive, and (3) combined. While previously believed to be "outgrown" by adulthood, current opinion indicates that many children will continue throughout life with symptoms that may affect both occupational and social functioning. Some medical researchers note that approximately 40%-50% of ADHD-hyperactive children will have (typically non-hyperactive) symptoms persist into adulthood.
What is the cause of ADHD?
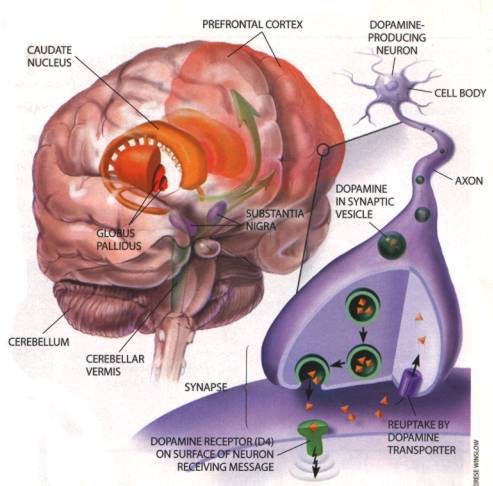
The cause of ADHD has not been fully defined. One theory springs from observations in functional brain imagining studies between those with and without symptoms. Similar variations have been shown in studies of the structure of the brain of affected and non-affected individuals. Animal studies have demonstrated differences in the chemistry of brain transmitters involved with judgment, impulse control, alertness, planning, and mental flexibility.
A genetic predisposition has been demonstrated in (identical) twin and sibling studies. If one identical twin is diagnosed with ADHD, there is at 92% probability of diagnosis with the twin sibling. When comparing nonidentical twin sibling subjects, the probability falls to 33%. (Overall population incidence is 8%-10% in the U.S., as described above.)
What are the symptoms of ADHD?
The diagnostic criteria for ADHD are outlined in the Diagnostic and Statistical Manual of Mental Health, 4th ed. (DSM-IV). All of the symptoms of inattention, hyperactivity, and impulsivity must have persisted for at least six months to a degree that is maladaptive and inconsistent with the developmental level of the child.
Inattention:
- The child often fails to give close attention to details or makes careless mistakes in schoolwork, work, or other activities.
- The child often has difficulty sustaining attention in tasks or play activities.
- The child often does not seem to listen when spoken to directly.
- The child often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (not due to oppositional behavior or failure to understand instructions).
- The child often has difficulty organizing tasks and activities.
- The child often avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort (such as schoolwork or homework).
- The child often loses things necessary for tasks or activities (toys, school assignments, pencils, books, or tools).
- The child is often easily distracted by extraneous stimuli.
- The child is often forgetful in daily activities.
Hyperactivity:
- The child often fidgets with his/her hands or feet or squirms in his/her seat .
- The child often leaves his/her seat in the classroom or in other situations in which remaining seated is expected.
- The child often runs about or climbs excessively in situations in which it is inappropriate.
- The child often has difficulty playing or engaging in leisure activities quietly .
- The child often talks excessively.
Impulsivity:
- The child often blurts out answers before questions have been completed.
- The child often has difficulty awaiting his/her turn .
- The child often interrupts or intrudes on others (for example, butts into conversations or games).
DSM-IV criteria for diagnosis of ADHD requires that some hyperactive, impulsive, or inattention symptoms that cause present difficulties were present before 7 years of age and are present in two or more settings (at school [or work] or at home). Similarly, there must be clear evidence of significant impairment in social, academic, or occupational functioning. In addition, symptoms may not entirely be caused by another severe physical disorder (for example, severe illness associated with chronic pain) or mental disorder (for example, schizophrenia, other psychotic disorders, severe disabling mood disorders, etc.).
Inattention symptoms are most likely to manifest about at 8 to 9 years of age and commonly are lifelong. The "delay" in onset of inattentive symptoms may reflect its more subtle nature (vs. hyperactivity) and/or variability in the maturation of cognitive development. Hyperactivity symptoms are usually obvious by 5 years of age and peak in severity between 7 to 8 years of age. With maturation, these behaviors progressively decline and often have been "outgrown" by adolescence. Impulsive behaviors are commonly linked to hyperactivity and also peak about 7 to 8 years of age; however, unlike their hyperactive counterpart, impulsivity issues remain well into adulthood. Impulsive adolescents are more likely to experiment with high-risk behaviors (drugs, sexual, driving, etc.). Impulsive adults have a higher rate of financial mismanagement (impulse buying, gambling, etc.).
How is ADHD diagnosed?
The evaluation of a child suspected of having ADHD involves various disciplines to provide a comprehensive medical, developmental, educational, and psychosocial evaluations. Interviewing parents and the child along with contact with the child's teacher(s) is crucial. Investigation regarding the family history for behavioral and/or social problems is imperative.
While direct person-to-person contact is considered vital at the outset of an investigation, follow-up studies may be guided by comparing standardized questionnaires (parental and teacher) completed prior to intervention and subsequent to therapeutic trials of medication, behavioral therapy, or other approaches. While there is no unique finding on physical exam in patients with ADHD, unusual physical features should prompt consideration of consultation with a geneticist due to the high association with ADHD behavioral patterns and well-recognized congenital syndromes (for example, fetal alcohol syndrome).
How are schools involved in diagnosing, assessing, and treating ADHD?
Physicians and parents should be aware that schools are federally mandated to perform an appropriate evaluation if a child is suspected of having a disability that impairs academic functioning. This policy was recently strengthened by regulations implementing the 1997 reauthorization of the Individuals With Disabilities Act (IDEA), which guarantees appropriate services and a public education to children with disabilities from ages 3 to 21. If the assessment performed by the school is inadequate or inappropriate, parents may request that an independent evaluation be conducted at the school's expense. Furthermore, some children with ADHD qualify for special-education services within the public schools, under the category of "Other Health Impaired." In these cases, the special-education teacher, school psychologist, school administrators, classroom teachers, along with parents, must assess the child's strengths and weaknesses and design an Individualized Education Program (IEP). These special-education services for children with ADHD are available though IDEA.
Despite this "federal mandate," the reality is that many school districts, because of underfunding or understaffing, are unable to perform "an appropriate evaluation" for all children suspected of having ADHD. The districts have the latitude to define the degree of "impairment of academic functioning" necessary to approve "appropriate evaluation." This usually means the children who are failing or near-failing in their academic performance. A very large segment of the ADHD-affected children will be "getting by" (not failing) academically (at least for their early years of school), but they are usually achieving well below their potential and will fall further behind each year on the academic prerequisite skills necessary for later school success. Thereafter, further educational testing may be requested from the school district. Unfortunately, some families will have to assume the financial burden of an independent educational evaluation. These evaluations are commonly done by an educational psychologist and may involve approximately eight to 10 hours of testing and observation spread out over several sessions. A primary goal of an educational evaluation is to exclude/include the possibility of learning disorders (such as dyslexia, language disorders, etc.).
Is ADHD inherited?
Research has shown that ADHD does seem to cluster in families. Several investigations have demonstrated that children who have ADHD usually have at least one close relative (child or adult) who also has ADHD. At least one-third of all fathers who have ADHD will produce a child with ADHD. With the newer realization that adults may also experience ADHD symptoms, it is not unheard of to have a parent's "problem at my job" be credited to
Is ADHD on the increase? If so, why?
No one knows for sure whether the prevalence of ADHD per se has risen, but it is very clear that the number of children identified with the disorder and who obtain treatment has risen over the past decade. Some of this increased identification and increased treatment seeking is due in part to greater media interest, heightened consumer awareness, and the availability of effective treatments. Teachers are better trained to recognize the condition and suggest that the family seek help, especially in the more mild to moderate cases. In addition, the diagnostic criteria for ADHD are now more specifically and concisely defined.
The diagnosis of ADHD is less of a social stigma than in the past. This more enlightened perspective reflects the understanding that ADHD is a biochemical disorder and not merely an "out of control child." As such, more parents are receptive to medical therapy for the condition rather than resorting to less effective home/school discipline techniques. Interestingly, the increase in prevalence of ADHD is not solely an American phenomenon but has been noted also in other countries. Whether the number of patients with ADHD has truly increased or rather better recognition and acceptance of ADHD as a diagnosis has "increased" remains to be further defined.
Can ADHD be seen in brain scans of children with the disorder?
Neuroimaging research has shown that the brains of children with ADHD differ fairly consistently from those of children without the disorder in that several brain regions and structures tend to be smaller. There is also a lack of expected symmetry between the right and left hemispheres. Overall, brain size is generally 5% smaller in affected children than children without ADHD. While this average difference is observed consistently, it is too small to be useful in making the diagnosis of ADHD in a particular individual. In addition, there appears to be a link between a person's ability to pay continued attention and measures that reflect brain activity. In people with ADHD, the brain areas that control attention appear to be less active, suggesting that a lower level of activity in some parts of the brain may be related to difficulties sustaining attention. It is important to reiterate that these laboratory observations are not yet sufficiently sensitive or specific enough to use to establish or confirm the diagnosis of ADHD or to monitor the effectiveness of treatment.
Can a preschool-aged child be diagnosed with ADHD?
The diagnosis of ADHD in the preschool-aged (under 5 years old) child is possible, but it can be difficult and should be made cautiously by experts well trained in childhood neurobehavioral disorders. A variety of physical problems, emotional problems, developmental problems (especially language delays), and adjustment problems can sometimes imitate ADHD in this age group. It is certainly not mandatory that the preschool-aged child showing ADHD-suggestive symptoms be placed in a preschool. The first line of therapy for children of this age showing ADHD-like symptoms is not stimulant medication therapy but rather environmental or behavioral therapy. This type of therapy can certainly be carried out in the home with appropriate training supplied to the parents. If the child is to be placed in a preschool, the caretakers must be equally trained in the techniques of behavioral therapy. Stimulant therapy can reduce oppositional behavior and improve mother-child interaction, but it's usually reserved for severe cases or when a child does not respond to environmental or behavioral interventions.
What is the impact of ADHD on children and their families?
Life can be hard for children with ADHD. They are often in trouble at school, can't finish a game, and have trouble making friends. They may spend agonizing hours each night struggling to keep their mind on their homework, only to forget to bring it to school. Family conflict can increase, placing added stress on exhausted parents and frustrated children. Adolescents are at increased risk for poor self-esteem, motor-vehicle accidents, tobacco and other drug use, early pregnancy, and lower educational attainment. School programs to help children with problems often connected to ADHD (social skills and behavior training) are not available in many schools. In addition, not all children with ADHD qualify for special-education services. To overcome these barriers, parents may want to look for school-based programs that have a team approach involving parents, teachers, school psychologists, other mental-health specialists, and physicians.
What is the role of alternative therapies in ADHD?
CAM (complementary and alternative medicine) therapies are considered and/or tried in over half of patients with ADHD. Many times, these modalities are used covertly and it is important for the treating physician to inquire about CAM to encourage open communication and review risks vs. benefits of such an approach. CAM treatment modalities incorporating vision training, special diets and megavitamin therapy, herbal and mineral supplements, EEG biofeedback, and applied kinesiology have all been advocated. The benefits of these approaches, however, have not been confirmed in double-blind controlled research studies. Families should be aware that such programs might require a long-term financial commitment that may not have insurance reimbursement as an option. Recent research on the benefits of specific polyunsaturated fatty acid (EPA and DHA) supplementation has demonstrated a therapeutic benefit in several well designed studies. Further research in this area will hopefully shed light on how these supplements work.
What are behavioral treatments?
In 2001, the American Academy of Pediatrics (AAP), in their Clinical Practice Guideline, suggested that when treating target ADHD symptoms, "clinicians should recommend stimulant medication and/or behavior therapy, as appropriate." Several forms of behavioral intervention have been found to show little or no effectiveness in treating ADHD patients. These included individual or play therapy, long-term psychotherapy, psychoanalysis, sensory-integration training, and cognitive behavioral therapy. However, one form of a non-medication approach, behavioral therapy, has been demonstrated to be somewhat effective with ADHD children. The therapy sessions are conducted by a mental-health professional (for example, a psychologist or social worker) and consist of parent and teacher training in child behavior management. The parents and teachers are taught to consider their child's behavior as a function of the disorder, rather than "bad behavior" or the result of failed parenting/teaching skills. The sessions then go on to teach the adults to pay attention to appropriate behavior, ignore minor inappropriate behavior, to give clear and concise directions, and to establish effective incentive programs, such as token or point reward systems. The adults manage misbehavior by applying immediate, specific, and consistent consequences (removal of privileges). Basically, the three principles of behavior therapy are
- 1. set specific goals,
2. provide rewards and consequences, and
3. keep using the rewards and consequences for a long time.
Parents can help their child's behavior with specific goals such as: (1) maintaining a daily schedule, (2) keeping distractions to a minimum, (3) setting small and reasonable goals, (4) rewarding positive behavior, (5) using charts and checklists to keep a child "on task," and (6) finding activities in which the child will succeed (sports, hobbies).
Many feel that behavior therapy can be an appropriate first-level treatment in several scenarios:
- 1. the milder ADHD patient,
2. for the preschool-aged child with ADHD-suspicious symptoms, and
3. when the family prefers this approach vs. medication.
What educational interventions have been studied and shown to be effective in the treatment of ADHD?
Children with ADHD may require adjustments in the structure of their educational experience, including tutorial assistance and the use of a resource room. Many children function well throughout the entire school day with their peers. However, some patients with ADHD will benefit from a "pull out session" to complete tasks, review specific homework assignments, and develop "management" skills necessary for higher education. Extended time for class work/tests may be necessary as well as assignments written on the board and preferential seating near the teacher. An IEP (individualized educational program) should be developed and reviewed periodically with the parents. ADHD is considered a disability falling under U.S. Public Law 101-476 (Individuals with Disabilities Education Act, "IDEA"). As such, individuals with ADHD may qualify for "appropriate accommodations within the regular classroom" within the public-school system. In addition, the Americans with Disabilities Act ("ADA") indicates that secular private schools may be required to provide similar "appropriate accommodations" in their institutions.
What medications are currently being used to treat ADHD?
Psychostimulant medications, including methylphenidate (Ritalin, Metadate, and Concerta), amphetamine (Dexedrine, Vyvanse, and Adderall), and atomoxetine (Strattera, marketed as a "non-stimulant," although its mechanism of action and potential side effects are essentially equivalent to the "psychostimulant" medications), a newer drug, are by far the most widely researched and commonly prescribed treatments for ADHD. Numerous short-term studies have established the safety and effectiveness of stimulants and psychosocial (behavioral therapy) treatments for not only alleviating the symptoms of ADHD but also improving the child's ability to follow rules and improve relationships with peers and parents. National Institute of Mental Health (NIMH) research has indicated that the two most effective treatment modalities for elementary-school children with ADHD are a closely monitored medication treatment or a program that combines medication with intensive behavioral interventions (behavior therapy). In the NIMH Multimodal Treatment Study for Children with ADHD (MTA), which included nearly 600 elementary-school children across multiple sites, nine out of 10 children improved substantially on one of these treatment programs.
Two types of antidepressant medications, the "tricyclic antidepressants" (TCA) (imipramine, desipramine, and nortriptyline) and bupropion (Wellbutrin), have also been shown to have a positive effect on all three of the major components of ADHD: inattention, impulsivity, and hyperactivity. They tend, though, to be considered as second options for the children who have shown inadequate response to stimulant medication or who experience unacceptable side effects from stimulant medication such as tics (uncontrolled movement disorders) or insomnia. The antidepressants, however, have a greater potential for side effects of their own, such as heart-rate and rhythm changes, dry mouth, headaches, and drowsiness, to name a few. If higher doses are required, bupropion may bring on seizures. The antidepressants, therefore, require more careful monitoring.
For the child who has a combination of ADHD and comorbid conditions such as depression, anxiety disorders, or mood disorders, stimulant medications can be combined with an antidepressant medication very successfully.
Are there standard doses for these medications?
For most children, stimulant medications are very safe and extremely effective. Research has shown that up to 80% of ADHD children show very good to excellent response to these medications. Improvements in the delivery systems for these medications in the last few years that have allowed the child to frequently only require one dose per day, alleviating the embarrassing "trip to the nurse's office" for a midday dose at school. Recently, a skin patch (Daytrana, a methylphenidate transdermal system) that, when applied daily, delivers the medication at a carefully controlled rate. The doctor will work with the child and his family to find the best medication, dosage, schedule, and delivery system. This requires careful individualization, since some children respond to one type of stimulant much better than another and each child's daily needs and schedules are so variable.
How long are children on these medications?
The expected duration of treatment has lengthened during this past decade as evidence has accumulated that benefits extend into adolescence and adulthood. Medication usage during the teen years can become problematic. The natural rebellion and desire for independence can make the adolescent protest against taking a medication. The need for a medication may reinforce anxiety that is common during the teen years in that it reinforces the notion of "I am different" to an age range that craves "fitting in." As such, parents and physicians must empower the teen to become a partner rather than a mere participant in his/her health. In some circumstances, it may even be necessary to allow the teenager to suffer the effects (academic and social) should he refuse to take medication. It is frequently the case that medication will be required into adulthood, and these years are critically important ones for the adolescent to begin to learn self-management of medication and other issues related to ADHD.
Hasn't the use of stimulant medication become excessive?
While it is certainly true that the prescribing of stimulant medication has increased sharply in the last 15 years, the statistics indicate that this increase coincides with the number of legitimately diagnosed cases of ADHD worldwide. Physicians, and the population in general, have achieved a much greater degree of awareness of and acceptance of the biological nature of ADHD, as well as the dramatic effectiveness of treatment protocols.
Are there differences in stimulant use across racial and ethnic groups?
There are significant differences in access to mental-health services between children of different racial groups, and consequently, there are differences in medication use. In particular, African-American children are much less likely than Caucasian children to receive psychotropic medications, including stimulants, for treatment of mental disorders.
Why are stimulants used when the problem is overactivity?
Recall that the three key components in ADHD are inattention, impulsiveness, and hyperactivity. While the exact nature of the disorder at the brain-cell level is not completely understood, it is felt that the medications work by stimulating the brain cells to make more of the chemicals (neurotransmitters) available that send messages from one brain cell to another. This improved message-sending system enhances the brains ability to pay attention, control behavior and impulses, plan actions, and follow through on schedules.
What are the risks of the use of stimulant medication and other treatments?
Stimulant medications have been successfully used to treat patients with ADHD for more than 50 years. This class of medication, when used under proper medical supervision, has an excellent safety record. In general, the side effects of the stimulant class of medications are mild, often temporary, and potentially reversible with adjustment in dosage amount or interval of administration. The incidence of side effects is highest when administered to preschool-aged children. Common side effects include appetite suppression, sleep disturbances, and weight loss. Less common side effects include an increase in heart rate/blood pressure, headache, and emotional changes (social withdrawal, nervousness, and moodiness). Patients treated with the methylphenidate patch (Daytrana) may develop a skin sensitization at the site of application. Approximately 15%-30% of children treated with stimulant medication develop minor motor tics (involuntary rapid twitching of facial and/or neck and shoulder muscles). These are almost always short-lived and resolve without stopping the use of medication.
A recent investigation studied the possibility of stimulant medication used to treat ADHD and cardiovascular side effects. Concern focused on a possible association with heart attack, heart-rate and rhythm disturbances, and stroke. At the time of the writing of this article, there is no certainty as to the relationship to these event (including sudden death) when medication is used in a pediatric population screened for prior cardiovascular symptoms or structural pathology. A positive family history for certain conditions (such as unusual heart-rhythm patterns) may be considered a risk factor. The current position of the American Academy of Pediatrics is that a screening EKG is not indicated before initiation of stimulant medication in a patient without risk factors.
Will children taking these medications for ADHD become drug addicts?
Although an increased risk of drug abuse and cigarette smoking is associated with childhood ADHD, this risk appears due to the ADHD condition itself, rather than its treatment. In a study jointly funded by the NIMH and the National Institute on Drug Abuse, boys with ADHD who were treated with stimulants were significantly less likely to abuse drugs and alcohol when they got older. Caution is warranted, nonetheless, as the overall evidence suggests that people with ADHD (particularly untreated ADHD) are indeed at greater risk for later alcohol or substance abuse. Because some studies have come to conflicting conclusions, more research is needed to understand these phenomena. Regardless, in view of the substantial, well-established findings of the harmful effects of inadequate treatment or no treatment for a child with ADHD, parents should not be dissuaded from seeking effective treatments because of misconstrued or exaggerated claims about substance-abuse risks.
"Diversion" is the transfer of medication from the patient for whom it was prescribed to another individual. Several large studies have indicated that 5%-9% of grade-school and high-school students and 5%-35% of college-age individuals reported use of non-prescribed stimulant medication. Approximately 16%-29% of students for whom stimulant medications were prescribed reported being approached to give, trade, or sell their medication. Misuse was more frequently seen in whites, members of fraternities and sororities, and students with a lower GPA. Diversion was more likely with the short-acting preparations. The most common reasons cited for use on non-prescribed stimulants were they "helped with studying," improved alertness, drug experimentation, and "getting high."
What is the relationship between ADHD and other disorders, such as learning disabilities, anxiety disorders, bipolar disorder, or depression?
While the recognition and understanding of ADHD has advanced greatly, it is still frequently under-recognized by most laypeople and many physicians that coexisting conditions affect as many as 50%-60% of all children with ADHD. Many of these coexisting conditions have many of the same symptoms of ADHD, and these symptoms are often the first signs of problems in youngsters under 5 years of age. At the time of the initial evaluation and diagnosis of ADHD, as well as throughout the lifetime of the ADHD patient, these other conditions must be looked for. They include:
Disruptive behavior disorders (in up to 35% of children with ADHD) include oppositional defiant disorder (ODD) and conduct disorder (CD). The behaviors in these areas go well beyond the usual "limit testing" of childhood and adolescence. Patients with ODD repeatedly demonstrate major defiance and hostility toward authority figures, refusal to follow rules, frequent loss of temper, deliberate annoyance of others, and generally angry, vindictive, and resentful behavior. Conduct disorder is more extreme and is defined as "a repetitive and persistent pattern of behavior in which the basic rights of others or major age-appropriate social rules are violated." CD extends into serious acts of violence against people and/or animals, school truancy, running away, vandalism, stealing, and so on. The person with CD is often labeled as "a delinquent" and has the potential for serious legal problems. It has been shown that early introduction of stimulant medication improves not only the basic ADHD symptoms but also the ODD or CD symptoms as well. Frequently, additional measures are also needed, especially in the CD category. These may include therapy from professional behavior-therapist intervention to special classrooms set up for more intensive behavior management to residential school placement with psychiatric involvement.
Mood disorders (in up to 15%-20% of children with ADHD) such as depression and bipolar disorder are often more difficult to recognize than the disruptive behavior disorders. Many children with ADHD alone are noted to be irritable, moody, easily frustrated, or immature emotionally. When these symptoms become severe enough to dominate the child's life, mood disorders must be considered. Children with combined ADHD/mood disorders (especially the more severe bipolar disorder) are at greater risk for drug abuse and suicide. Children in this category often require referral to a developmental/behavioral specialist or a psychiatrist, as there are a variety of behavioral/psychotherapic methods along with additional medications that can be very helpful.
Anxiety disorders (in up to 25% of children with ADHD) often involve symptoms that are largely internal and, again, more difficult to immediately recognize. These symptoms may be extreme fear, worry, and feelings of panic associated with physical findings like racing heart rates, muscle tension, nausea, vomiting, or extreme sweating. These bouts of anxiety are severe, ongoing, and frequent (at least three to five times per week and lasting for more than one hour). The use of stimulant medication alone may help both the ADHD symptoms and anxiety symptoms as well. If not, behavioral therapy and/or additional medication in the tricyclic antidepressant family or the selective serotonin reuptake inhibitor (SSRI) family (Celexa, Zoloft, Lexapro, and Prozac, etc.) can be very helpful.
Learning disorders are conditions that can interfere with the child's mastery of specific skills like mathematics or reading. They can include auditory perceptual problems, visual perceptual problems, and so on. The school should be approached to carry out testing for these specific learning disorders. Depending on the type of learning disorder detected, altering teaching techniques can help the student bypass areas of weakness and utilize other pathways of learning that may actually be quite strong.
What is the prognosis for individuals with ADHD?
Research supports the clinical observation that as many as 50% of children with ADHD will have symptoms persist into adulthood. One caveat needs to be
- Education: Follow-up studies of children with ADHD growing into adolescence showed impairment of academic success. A few studies into adulthood have demonstrated persistence of these findings. Completion of expected schooling, lower achievement scores, and failure of courses are areas of concern.
- Employment: The rate of adult employment of those with and without a diagnosis of ADHD did not vary; however, those with ADHD did have occupations with a lower "job status."
- Socialization issues: As noted above, a significant subset of children with ADHD has an accompanying disruptive behavior disorder (ODD and CD). In studies that followed children with ADHD into adulthood, between 12%-23% have socialization problems (vs. 2%-3% of the general population).
- Substance abuse: The medical literature investigating whether those with ADHD have a higher likelihood for such high-risk behaviors is controversial. The largest study to date supports other smaller studies that indicate ADHD patients who consistently take their medication have twice the likelihood not to utilize drugs or excessive alcohol.
- Driving: Teens with ADHD are two to four times more likely to have motor-vehicle accidents or have their license suspended than peers without such a diagnosis. Impulsivity and inattention again seem to be limited when at-risk teens consistently take their recommended medication.
What is the history of ADHD? How is it related to ADD?
ADHD has assumed many aliases over time from hyperkinesis (the Latin derivative for superactive) to hyperactivity in the early 1970s. In the 1980s, DSM-III dubbed the syndrome attention deficit disorder (or ADD), which could be diagnosed with or without hyperactivity. This definition was created to underline the importance of the inattentiveness or attention deficit that is often but not always accompanied by hyperactivity. The revised edition of DSM-III, the DSM-III-R, published in 1987, returned the emphasis back to the inclusion of hyperactivity within the diagnosis, with the official name of ADHD. With the publication of DSM-IV, the name ADHD still stands, but there are varying types within this classification to include symptoms of both inattention and hyperactivity-impulsivity, signifying that there are some individuals in whom one or another pattern is predominant (for at least the past six months). In the International Classification of Diseases (used predominantly in other Western countries), the term hyperkinetic disorder is used, but the criteria are the same as for ADHD/combined type.
What are the future research directions for ADHD?
- 1. The current criteria for the diagnosis of ADHD are taken from the Diagnostic and Statistical Manual of Mental Health Disorders, 4th ed. (DSM-IV) published in 1994. Much has been revealed about ADHD since then. The next edition (DSM-V expected May 2012) will need to reflect our broader understanding of ADHD. In addition, there is currently just one set of diagnostic criteria used for the diagnosis of ADHD for all age groups. Clearly, we must establish different diagnostic criteria for childhood, adolescent, and adult ADHD.
2. We need more data regarding the long-term effects of the methods of treatment (medication, behavioral therapy, etc.) that have now been used for several decades, as well as the long-term outcome of children with ADHD that have not been treated.
3. The development of psychotropic medications in non-ADHD areas has expanded dramatically in the past few years. We must continue to look for even safer and more effective medications for ADHD alone, and (perhaps even more importantly) for the patients with combined ADHD/comorbid conditions.
4. The societal impact of ADHD needs to be investigated. Studies in this regard include: strategies for implementing effective medication management or combination therapies in different schools and pediatric health-care systems; the nature and severity of the impact on adults with ADHD beyond the age of 20, as well as their families; and determination of the use of mental-health services related to diagnosis and care of people with ADHD.
5. Additional studies are needed to improve communication across educational and health-care settings to ensure more systematized treatment strategies.
6. Studies should be done in the areas of prevention/early intervention strategies that target known risk factors that may lead to later ADHD.
7. Further evaluation is necessary for the rapidly evolving technology of brain-imaging techniques as a possible tool in the diagnosis and subsequent management of ADHD.
Attention Deficit Hyperactivity Disorder (ADHD) At A Glance
- ADHD refers to a chronic disorder that initially manifests in childhood and is characterized by hyperactivity, impulsivity, and/or inattention.
- The cause of ADHD has not been fully defined and may involve brain-chemical and genetic factors.
- The diagnosis of ADHD involves many disciplines to include comprehensive medical, developmental, educational, and psychosocial evaluations.
- ADHD can cluster in families.
- Children with ADHD may require adjustments in the structure of their educational experience including tutorial assistance and the use of a resource room.
- Medications are available to treat ADHD and can improve overall function.
For more information regarding attention deficit disorder, contact the local school-district office or one of the following:
Bureau of Education for the Handicapped
U.S. Office of Education
Washington, DC 20202
The Association for Children With Learning Disabilities, Inc.
3739 S. Delaware Place
Tulsa, OK 74105 
Council for Exceptional Children
PO Box 9382 Mid-City Station
Washington, DC 20005
U.S. Office of Civil Rights
Washington, DC 20402
For more information about ADHD, please visit C.H.A.D.D. (Children and Adults with Attention-Deficit/Hyperactivity Disorder (http://www.chadd.org).
Portions of the above information were provided with the kind permission of the National Institute of Mental Health (http://www.nimh.nih.gov).
|
Bookmark this post:
|
|

0 comments
Post a Comment