
What is concussion and what causes concussion?
Mild traumatic brain injury, or concussion, can be defined as a short-lived loss of brain function due to head trauma that resolves spontaneously. With concussion, function may be interrupted but there is no structural damage to the brain.
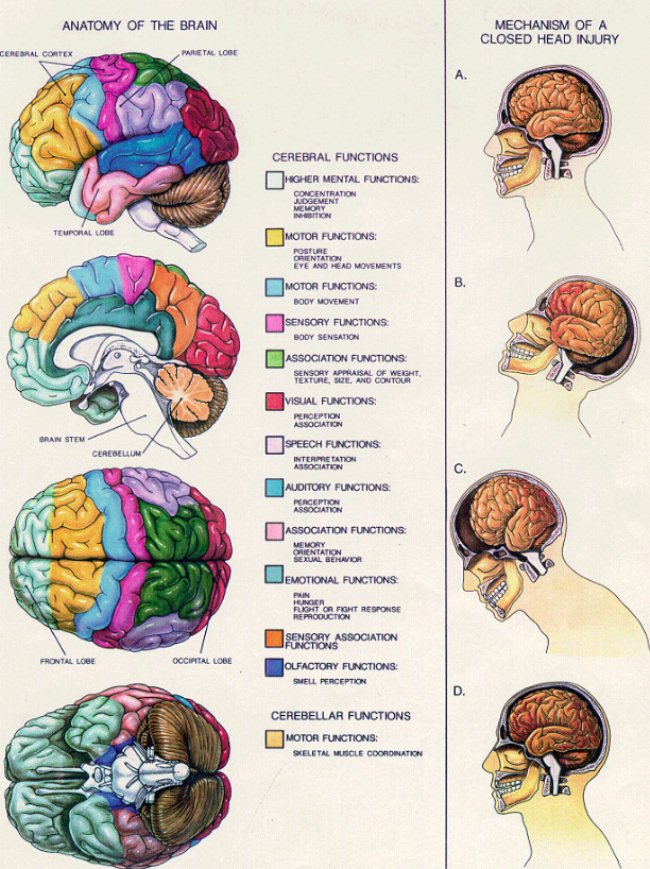
The brain floats in cerebrospinal fluid and is encased in the skull. These protections allow it to withstand many of the minor injuries that occur in day to day life. However, if there is sufficient force to cause the brain to bounce against the rigid bones of the skull, then there is potential for injury. It is the acceleration and deceleration of the brain against the inside of the skull that can cause the brain to be irritated and interrupt its function. The acceleration can come from a direct blow to the head or face, or from other body trauma that causes the head to shake. While temporary loss of consciousness due to injury means that a concussion has taken place, most concussions occur without the patient being knocked out. Studies of football players find that the majority aren't aware that they had sustained a head injury.
Picture of the brain and potentially brain injury areas

What are the types of concussion?
Historically, attempts to classify the severity of concussion were based on the loss of consciousness and its duration, and the presence of amnesia. It was presumed that there was a correlation between those two events and the amount of potential brain damage. The International Conference on Concussion in Sports recommended that concussion be divided into two groups: simple and complex.
- Simple concussion: In a simple concussion, the person the symptoms gradually resolve, and the patient returns to normal function in 7 - 10 days.
- Complex concussion: In complex concussions, symptoms persist and thought processes are affected. Patients with repeated concussions would fall into the complex category.
What are the signs and symptoms of concussion?
The signs and symptoms of concussion may be obvious or subtle. Much of the experience in caring for mild head injuries comes from the treatment of sports injuries. Football, hockey, and soccer have high potential for head injury, and player research has given insight into what symptoms may occur.
While dramatic, loss of consciousness or seizure are not common in concussion and do not predict severity. More common are mild confusion and disorientation. Symptoms tend not to be objective and may be hard to describe. As well, they may be delayed for many hours after injury, and sometimes the initial injury may have been forgotten or discounted.
Typical symptoms of concussion include:
- Headache
- dizziness
- Nausea
- Dazed feeling
- Visual symptoms
- Irritability
Physical Signs
Since, by definition, concussion does not damage the structure of the brain, the physical examination should be normal. More subtle findings may include:
- Slow to answer questions or follow directions
- Poor concentration
- Emotional lability (emotional changes or instability)
- Slurred speech
- Personality changes
How is concussion diagnosed?
Physical Examination and Testing
History and physical examination are crucial to making the diagnosis of concussion. Understanding the mechanism of injuries allows the healthcare provider to decide if further radiologic testing is required. A normal neurologic examination is somewhat reassuring that no major structural injuries to the brain have occurred.
Glasgow Coma Score (GCS)
The GCS was developed to quickly assess a patient's neurologic status based on speech, eye opening, and movement. The scale is used as part of the initial evaluation of a patient. Since it "scores" the level of coma, the GCS can be used by healthcare providers with different skill levels to assess changes in patient status.
| Glasgow Coma Scale | |
| Eye Opening |
|
| Spontaneous | 4 |
| To loud voice | 3 |
| To pain | 2 |
| None | 1 |
|
| |
| Verbal Response |
|
| Oriented | 5 |
| Confused, Disoriented | 4 |
| Inappropriate words | 3 |
| Incomprehensible words | 2 |
| None | 1 |
|
| |
| Motor Response |
|
| Obeys commands | 6 |
| Localizes pain | 5 |
| Withdraws from pain | 4 |
| Abnormal flexion posturing | 3 |
| Extensor posturing | 2 |
| None | 1 |
Computerized Tomography (CT scan)
Not everyone who has sustained a blow to the head needs a CT scan. The Canadian Head CT Rules were developed to minimize the number of brain scans that were done with little chance of finding bleeding in the brain and requiring an operation. There is no need for CT scanning if none of the following high or medium risk criteria are met.
High risk for bleeding:
- Glasgow Coma Score <15>
- Suspected open or depressed skull fracture
- Any sign of basal skull fracture [blood behind the eardrum, "raccoon eyes" or bruising around the eyes, cerebrospinal fluid leaking from the nose or ears, or Battle's sign (bruising behind the ear)]
- More than two episodes of vomiting
- Age > 65 years
Medium risk for bleeding:
- Amnesia before impact >30 minutes - This refers to loss of memory prior to the trauma (retrograde amnesia).
- Amnesia can be retrograde (loss of memory of events prior to the injury) and antegrade (where the person cannot remember events that have occurred after he injury). Antegrade amnesia is common and not an indicator of significant brain trauma. Retrograde amnesia of more than 30 minutes is a risk for brain bleeding.
- Amnesia can be retrograde (loss of memory of events prior to the injury) and antegrade (where the person cannot remember events that have occurred after he injury). Antegrade amnesia is common and not an indicator of significant brain trauma. Retrograde amnesia of more than 30 minutes is a risk for brain bleeding.
- Dangerous mechanism of injury (pedestrian struck by motor vehicle, occupant ejected from motor vehicle, fall from height >3 feet or five stairs)
These indications are valid for those patients aged 2 to 65.
X-rays of the skull are not indicated in minor head trauma, since normal x-rays do not correspond to a normal brain.
Since concussion is defined as a temporary change in brain function, it is important to examine the patient on more than one occasion. Brain function may or may not correlate with the resolution of symptoms. Neuropsychologic testing can be used to assess brain function to decide when to allow a patient to return to full activity.

What is the treatment for concussion?
Time is the ally in concussion treatment since most symptoms resolve within a week to 10 days. Treatment is directed at symptom control for headaches, nausea, dizziness, and insomnia. Discussion with employers may be needed to alert them to issues of poor work performance due to difficulty with concentration and comprehension.
How can concussion prevented?
As with most accidents, injury prevention is the first consideration. The following are all important steps to prevent concussion and severe head injuries:
- workplace safety using helmets where required or recommended;
- using seatbelts in motor vehicles;
- wearing helmets while bicycling and motorcycle riding; and
- recreational athletes should use head protection appropriate for their sport.
What is the future of concussion?
Newer computer-based testing products, like ImPACT™, may be able to predict when athletes can return safely to the field of play. The test requires a baseline measurement of the athlete's mental function and after injury can determine when the athlete's brain has returned to normal. It may be able to replace neuropsychologic testing, which is time intensive and not always available to the general population.
There are certain genes that predispose to poor outcome after minor head injury. Genetic issues that may presdispose to poor outcome involve abnormal swelling of the brain in the early stages of concussion, while late complications may be related to chronic destruction of brain tissue.
References:
Summary and Agreement Statement of the 2nd International Conference on Concussion in Sport, Prague 2004. Clin J Sport Med. Volume 15, Number 2, March 2005
Stiell IG, et al. The Canadian CT head rule for patients with minor head injury. Lancet May 5, 2001;357:1391-6.
ImPACT™ (http://www.impacttest.com/index.php)
Kors E, Terwindt G, Vermeulen F, et al. Delayed cerebral edema and fatal coma after minor head trauma: Role of the CACNA1A calcium channel subunit gene and relationship with familial hemiplegic migraine. AnnNeurol. 2001;49:753-760.
Teasdale G, Nicol J, Murray G. Association of Apolipoprotein E polymorphism with outcome after head injury. Lancet. 1997;350:1069-1071.
sourceLast Editorial Review: 1/4/2008
|
Bookmark this post:
|
|

0 comments
Post a Comment