
Introduction
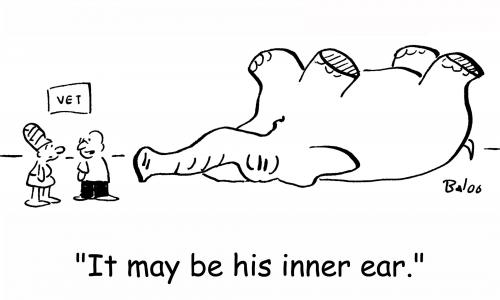
Ponder this: if a cat is dropped upside down, it will land right side up on all four paws. If a newborn infant is tilted backward, its eyes will roll downward so that its gaze remains fixed on the same point. If, as you read this article, you shake your head rapidly from side to side, the print nonetheless will stand still. Each of these scenarios is an example of how a healthy balance (vestibular) system compensates for daily changes in our spatial orientation.
Balance is a state of body equilibrium or stability. We often take for granted how dependent we are on a healthy balance system. When the system breaks down, however, patients will describe symptoms such as dizziness, vertigo, lightheadedness, or motion sickness.
How do patients describe the symptoms caused by balance disorders?
More than two million people per year visit their doctor for vestibular balance disorders.
These disorders are the ninth most common complaint that leads patients to visit their primary care physicians. Furthermore, it is one of the most common reasons elderly people seek medical advice.
Patients often describe balance problems in terms of vertigo, dizziness, lightheadedness, and motion sickness. But, not all of these symptoms are always caused by disorders of the vestibular system. Moreover, although one person may describe a balance problem using one or more of these terms, another person may use a different combination of these terms to describe the very same condition. In fact, some people will even use the word dizziness to indicate that they simply do not feel well. It is important, therefore, for patients to not use general terms when describing their balance problems. Put another way, it is best for patients to simply describe the sensation they feel without using general terms like dizziness or vertigo.
Dizziness
In general, physicians refer to dizziness as a feeling of being woozy, drunk, unsteady, or giddy. There is often a feeling of imbalance (disequilibrium) without a true sensation of turning or spinning. Dizziness is a general-purpose, rather imprecise term used to describe the sensation of imbalance (sensory disorientation). Although patients often use the word dizziness to describe balance or inner ear problems, it is typically not caused by a disorder of the inner ear.
Vertigo
Vertigo refers to an hallucination of motion that can be linear (straight ahead), falling, or rocking. It is often described as a spinning, turning, or whirling sensation. What's more, the spinning may be one of self-rotation (subjective vertigo) or rotation of the surrounding environment (objective vertigo). In most cases, the symptom of vertigo implies a disorder of the inner ear or vestibular system.
Lightheadedness
Lightheadedness refers to the typical sensation one experiences prior to a fainting episode. Associated symptoms can include sweating, feeling cold, shortness of breath, numbness around the mouth or of the fingers, and a dimming or tunneling of vision. Lightheadedness is caused by a momentary decrease in blood flow to the brain. This sensation can occur for a number of reasons including medication side effects and heart (cardiac) and blood vessel (vascular) problems. For instance, orthostatic hypotension is low blood pressure that occurs upon standing. In this condition, the low blood pressure decreases blood flow to the brain, and thereby, causes lightheadedness.
Contrary to popular belief, high blood pressure (hypertension) itself does not cause lightheadedness. Hypertensive patients may experience lightheadedness, however, when their blood pressure drops for any reason. It happens that the most common reason for such a drop in blood pressure is a response to their blood pressure medications. Lightheadedness is usually not a common complaint from patients with vestibular problems.
Motion sickness
Whereas vertigo, lightheadedness, and dizziness are symptoms of diseases, motion sickness is a normal response to an abnormal situation. It is a general term that includes such conditions as seasickness, airsickness, carsickness, and even space sickness. Motion sickness is caused by a real or perceived motion stimulus to which a person has not yet adapted. It occurs when conflicting information is fed into the vestibular and other sensory systems.
Individual thresholds (the amount of motion it takes) to trigger motion sickness differ. Eventually, however, anyone will develop motion sickness if placed in a situation that provides enough motion. The symptoms of motion sickness include nausea, vomiting, spinning, sweating, and headache. In fact, motion sickness has ruined many a vacation, and has limited the activities or even incapacitated those who are prone to it. (Motion sickness is discussed in more detail below.)
What problems cause balance disorders?
The cause of a balance disorder may be a well-defined anatomical condition, or simply a psychological reaction to an unpleasant life event. In some situations, the underlying condition is of only minor significance, while at other times it may be life threatening. Unfortunately, finding the cause of a balance problem can at times be frustrating and exhausting. For example, almost any problem in any system of the body can lead to the symptom of dizziness or to a balance disorder.
Our orientation in space and, therefore, our balance or equilibrium, is primarily measured by three sensory systems:
- The eye (visual) system
- The balance (vestibular) system of the inner ear
- The general sensory system including motion, pressure, and position (proprioception) sensors in joints, muscles, and skin.
These three systems continuously feed information to the brainstem and brain about our position in space relative to gravity. (The brainstem is the part of the brain that connects to the spinal cord.) The brain, in turn, processes these data and subsequently uses the information to make minute adjustments of our head, body, joints, and eyes. When all three sensory systems and the brain are properly functioning, the final result is a healthy balance system.
By the same token, when the balance system is not functioning, one can usually trace the problem back to a disorder of one of the three sensory systems or the data processor (brain). The problems in each of the following areas correspond to one of these sensory systems or the brain.
Visual
Visual input provides essential clues about our spatial orientation. That is, visual input tells the brain where the body is "in space:" what direction it is pointing, what direction it is moving, and if it is turning or standing still. Also, something as simple as walking a straight line is much easier if we can see our surroundings. Feeling seasick is a problem resulting from a miscommunication between a healthy visual system and a healthy inner ear (vestibular) system. In this circumstance, the ears are telling the brain that there is movement, while the eyes may be seeing the fixed surroundings of the cabin. Simple eye refraction errors, glaucoma, and cataracts are examples of visual problems that in some individuals may be enough to give them a balance disorder.
Inner ear (vestibular)
Just where is the inner ear? Also known as the labyrinth, the inner ear is located deep to the outer ear and middle ear, and is encased within the so-called petrous portion of the temporal bone of the skull. The figure below is a diagram showing the parts of the ear. 
Figure 1. Diagram of outer, middle, and inner ear. The outer ear is labeled in the figure and includes the ear canal. The middle ear includes the eardrum (tympanic membrane) and three tiny bones for hearing. The bones are called the hammer (malleus), anvil (incus), and stirrup (stapes) to reflect their shapes. The middle ear connects to the back of the throat by the Eustachian tube. The inner ear (labyrinth) contains the semicircular canals and vestibule for balance, and the cochlea for hearing.
The vestibular structures of the inner ear are the vestibule (which is made up of the utricle and saccule) and the three semicircular canals. These structures work somewhat like a carpenter's level (a tool used to show how "level" a horizontal or vertical surface is). That is, they work by way of the vestibulocochlear nerve with the vestibular center in the brain to deal with body balance and position. (The rest of the inner ear, that is, the cochlea, is concerned with hearing.) Thus, the vestibular system includes the vestibule, the semicircular canals, the vestibular branch of the vestibulocochlear nerve, and the vestibular center in the brain.
The vestibular system measures linear and rotational movement. A number of disorders can cause this system to stop working or provide inappropriate information. These disorders include Meniere syndrome, labyrinthitis, benign paroxysmal positional vertigo, ear infections, tumors, or trauma. Each of these conditions is discussed below.
General sensory system
The general sensory system consists of motion, position, and pressure sensors in the skin, muscles, and joints. These sensors provide important touch (tactile) and position information to keep us balanced. For example, if someone pushes you from behind, a slight increase will occur in the activity of the pressure sensors in the ball of the feet. As these sensors note the increased pressure, the brain is notified, and it knows from experience that the body is being pushed forward. The brain then uses this information to tell the body to shift a small amount of weight backward to prevent the body from toppling forward. So, disorders involving the general sensory system can result in balance problems.
Brain
As mentioned, the brain processes the information from the three sensory systems. Any problem that interferes with the proper functioning of the central nervous system (CNS), therefore, can lead to a balance disorder. (The CNS is made up of the brain and spinal cord.) Unlike the problems associated with the three sensory input systems discussed above, however, with CNS problems, it is unusual to have vertigo as the only symptom.
Examples of processor problems include brain infections or abscesses, strokes (vascular insufficiency), migraine headaches, brain tumors, head trauma, degeneration syndromes (due, for example, to alcoholism), and multiple sclerosis. Furthermore, any disease that interferes with the proper functioning of the CNS can also cause balance problems. Examples of these diseases include heart conditions (e.g., abnormal heart rhythms or congestive heart failure), anemia, metabolic or hormonal conditions (diabetes, dehydration, or thyroid disorders), and psychological problems, such as anxiety or heavy breathing (hyperventilation).
A common cause of this type of balance problem is insufficient blood flow to the brain. In elderly individuals, there is often narrowing of the blood vessels to the brain (hardening of the arteries or arteriosclerosis) or decreased blood flow from the heart (e.g., with heart failure). In these situations, because of decreased blood flow to the brain, the affected individual will become dizzy when getting up from a sitting or reclining position.
Since the balance system has so many components with interdependent functions, it is not surprising to find literally hundreds of different causes of balance problems. Although it may not be possible to diagnose the exact cause of imbalance in every patient, a patient's symptoms often can be classified into a well-defined clinical disorder.
How are patients with balance disorders evaluated?
The most important part of the evaluation is the patient's description of the symptoms of the balance disorder. As already mentioned, it is important for the patient to describe the details of what they are experiencing, and try to avoid using general terms such as dizzy or vertigo. What's more, the doctor will ask other important questions as well. For example, how long and how often have they had the problem? Does the symptom of the balance problem occur in attacks or is it constant? Is it triggered by movement or by arising from a sitting or lying position? Is it associated with other symptoms such as hearing loss, ringing of the ears (tinnitus), ear fullness, nausea, or vomiting? Have there been any general health changes, new medications, recent head trauma, or recent or current infections. Are there any other neurological symptoms, such as weakness, vision problems, or tingling?
It is important to explore any factors that trigger and cause the balance disorder. Specifically, these factors might include change of body position, relation to movement, and association with stress or hyperventilation. For example, vertigo that occurs while turning in bed is typical of benign positional vertigo. In contrast, lightheadedness brought on by getting up quickly from a lying or sitting position is typical of a condition called orthostatic (positional) hypotension (low blood pressure). And, emotionally triggered attacks may be associated with anxiety or hyperventilation.
The duration of an attack of vertigo is very helpful in determining the cause. For example vertigo that follows head movement and lasts less than a minute is typical of benign positional vertigo. But an attack of vertigo lasting hours is more commonly due to Meniere disease. Constant vertigo, however, is typically not an inner ear disorder, but more commonly is a central nervous system problem.
A general physical examination of the ears, head, and neck should be done with special emphasis on tests of balance function. Additional testing is often recommended such as hearing tests, CT scans, MRI scans (magnetic resonance imaging), electronystagmography (ENG), and blood tests. ENG is a technique to measure involuntary eye movements (nystagmus) that are related to balance disorders. In some situations, referral to an ear specialist (otolaryngologist) or neurologist may also be necessary. In addition, consultations with a cardiologist, psychiatrist, and general internist are often indicated.
What general advice can be given to patients with balance disorders?
Balance disorders can often be very unpredictable. Depending on the cause, the symptoms can occur at any time, even after long periods of absence of symptoms (remission). It is important, therefore, to take proper precautions in order to avoid accidents that could be caused by a balance disorder. The following is a list of general recommendations for people with balance disorders:
- Change your position slowly, especially when going from a lying down or sitting to a standing position. When you get out of bed, sit on the side of the bed for several minutes to gain your orientation and allow your circulatory system to adjust.
- When walking, focus on distant objects. Do not look down at your feet. Avoid walking in dark areas or on unstable ground.
- When riding in a car, try to sit in the front seat. Look out the window at a fixed point. When going around curves, look at a distant object beyond the curve.
- Maximize the function of other sensory systems, such as hearing and sight. Investigate the need for new glasses or hearing aids.
- Use a cane, walking stick, or walker for support and to give additional pressure and touch (tactile) orientation.
- If you are having attacks of dizziness, do not drive or operate machinery until your doctor says it is safe to do so. Avoid climbing ladders or other situations that may be dangerous should you suddenly feel dizzy.
- Be especially cautious when using medications that may cause balance problems as a side effect.
How are balance disorders treated?
The treatment of a balance or vestibular disorder will depend on its cause. Accordingly, specific medicinal (pharmacological) and surgical treatments are discussed below with each specific disease process. In general, however, symptomatic control of vertigo, regardless of the cause, can often be accomplished with diazepam (Valium) given intravenously or orally. The accompanying nausea and vomiting can be treated with droperidol (Inapsine), promethazine (Compazine), prochlorperazine (Phenergan), or ondansetron (Zophren). Fluid and electrolyte replenishment is often very helpful, and can be provided orally or if necessary, intravenously.
What are vestibular rehabilitation exercises?
Once the short-term (acute) symptoms of a balance disorder have subsided, physical therapy (that is, vestibular rehabilitation exercises) can be particularly helpful. The goal of this rehabilitation is to help the patient adjust (accommodate) to the balance problem so as to diminish recurrent symptoms. The following is a list of vestibular exercises that may be helpful.
1. Seated or in bed.
- Eye movements: move the eyes slowly at first, then quickly up and down, side to side, and diagonally. Focus on your finger as you move it from 1 foot to 3 feet away from the face.
- Head movements: move the head slowly at first, then quickly, with eyes open, bending forward and backward, turning from side to side, tilting from side to side, and moving diagonally. Repeat with the eyes closed.
- Repeat section 1 exercise while standing.
- Change from a sitting to a standing position, first with eyes open, and then with the eyes closed.
- Throw a ball from hand to hand above eye level.
- Throw a ball from hand to hand under the knees.
- Change from sitting to standing, turning first to one side and then to the other.
3. Moving about
- Walk across the room with eyes open, and then with eyes closed.
- Walk up and down a slope with eyes open, and then with eyes closed.
- Walk up and down steps with eyes open, and then with eyes closed.
- Sit up and lie down in bed
- Sit down in a chair, then stand up
- Recover balance when pushed in a specific direction.
- Throw and catch a ball
- Engage in any game involving stooping or stretching and aiming, such as bowling, volleyball, or shuffleboard.
What are the specific balance disorders and their treatments?
Meniere disease
Please read the main article on Meniere disease for information about this condition.
Motion sickness syndrome
Motion sickness syndrome includes such conditions as seasickness, airsickness, carsickness, and space sickness. Common to all of these is the presence of a motion or visual stimulus to which a person has not adapted. Symptoms include dizziness, increased perspiration, hyperventilation, nausea, vomiting, decreased appetite, increased salivation, and vague discomfort (malaise). Individual responses to the same situation are quite variable. In severe situations, however, even the most seasoned sailor can and will get seasick.
Motion sickness results from a conflict between the balance (vestibular) and eye (visual) systems. For example, if a person sits in an enclosed cabin on a ship at sea, the person will see a stationary environment but the vestibular system will be measuring constant movement. In this case, the continued motion of the head, as measured by the vestibular system, is not accompanied by a commensurate motion of the visual scene. At this point, therefore, a conflict exists between the two sensory structures, the eyes and the ears. If the person goes outside and looks at the horizon, however, the match between the visual and vestibular signals is in more alignment, and seasickness improves. Similarly, when riding in a car, sitting in the front seat allows ample peripheral vision of the surrounding stationary structures.
Motion sickness can also occur in the absence of movement. For example, an amusement type motion simulator or cinema movies can induce symptoms of motion sickness. In these situations, motion sickness occurs because the visual system perceives motion but the vestibular system does not detect motion. Again, there is a conflict between the vestibular and visual systems.

Space sickness is another kind of motion sickness, which is brought on by active head movement in space. In fact, space sickness has been reported in 50% of astronauts. It usually resolves within 2-3 days of space travel. As you might expect, lack of gravity appears to be the activating force in space sickness. The problem is thought to occur because the saccule and utricle in the vestibule measure the effect of both linear acceleration and gravity. On earth, therefore, a specific head movement will generate a well-defined response, while in space (the absence of gravity), the same head movement will produce a different response. After several days in space, however, most astronauts will recalibrate their vestibular systems to account for the absence of gravity. But then, on return to a gravity environment, astronauts often will develop transient motion sickness until they can adjust back to functioning in gravity again.
Another important feature of motion sickness is the adaptation process. Adaptation occurs with continual exposure to the motion that causes the motion sickness. So, it is not unusual for someone to feel seasick the first day out at sea. But then they adapt to the continued motion and no longer have symptoms of motion sickness. On the other hand, the mal de debarquement syndrome is a persistent sensation of motion after return to a stable environment. Thus, until the vestibular system is able to readapt itself, individuals often report the feeling of motion for several hours to days after disembarking from a sea voyage.
Motion sickness can occur at any age, although its frequency increases after age 40. Interestingly, children under two years of age appear to be highly resistant to motion sickness. A resistance or particular response to one form of motion sickness does not grant resistance or predict a response to other forms of motion sickness. Psychological factors may also play a role in the development of motion sickness.
How is motion sickness treated?
Multiple medications and home remedies have been touted as a cure for motion sickness. Unfortunately, however, few medications are effective, and none affords complete protection. Medications that do not require a prescription include dramamine and meclizine (Bonine, Antivert). Prescription medications include tranquilizers, anti-depressants, and anti-nausea medications. Scopolamine is used as a patch scopolamine (Transderm Scop) applied to the skin behind the ear. Scopolamine patches are safe and effective and can provide protection for up to three days. In the elderly, however, they can cause psychological problems as side effects.
All motion sickness medications work by diminishing activity at the vestibular center (nucleus) in the brain. They thereby diminish the potential for eye-balance (visual-vestibular) conflict. Motion sickness is usually a self-treatable problem. In severe and progressive cases, however, medical evaluation should be undertaken.
Vestibular migraines
Dizziness as a symptom of migraine is a common and often ignored cause of balance disorders. Migraine is a blood vessel (vascular) disease characterized by periodic, usually one-sided, headaches. These headaches are often preceded for a variable time by associated neurological symptoms, called the aura. Dizziness and vertigo can occur in individuals with migraine as part of the migraine aura or separately. Furthermore, dizziness may not occur at the same time as the headache and can even occur as an isolated event. Particularly in younger patients, dizziness or vertigo may predate the onset of headaches entirely.
A family history of migraine is very common. Indeed, a family history of migraine should alert a person that a balance disorder may be migraine related. Migraine is estimated to affect nearly 25% of women, 15% of men, and 5% to 10% of children. Vertigo is very common in persons with migraine, occurring in about 25% of them. Actually, in one series, 42% of migraine patients experienced vertigo not in association with their headaches.
The management of migraine is divided into two categories: symptomatic and preventive treatments. Acute attacks can be treated and stopped (aborted) with various medications including Fiorinal, Midrin, and sumatriptan (Imitrex). Preventive treatment is most frequently accomplished with propranolol (Inderal). Amitriptyline, calcium channel blockers, and acetazolamide (Diamox) are also used. Acetazolamide has been particularly effective in treating patients with vestibular symptoms associated with migraine. For more please read the Migraine Headache article.
Inner ear trauma
Trauma to the inner ear can occur from penetrating injuries, blunt skull trauma with skull base (temporal bone) fracture, concussion damage to the inner ear, and sound or pressure trauma (barotrauma). The ear trauma itself can cause balance symptoms. But, in addition, head trauma can dislodge particulate matter that becomes free floating within the inner ear and causes positional vertigo (see benign paroxysmal positional vertigo in this article). Treatment is directed toward the underlying injury. Vestibular rehabilitative therapy is often helpful.
Perilymphatic fistula
The perilymphatic fluid baths the membranous structures (vestibule, semicircular canals, and cochlea) of the inner ear. (These structures are filled with another fluid called the endolymph.) A perilymphatic fistula occurs when there is leakage of the perilymphatic fluid from a hole between the inner ear compartment and the middle ear or mastoid. This hole can result from surgery, trauma, infection, developmental (before birth) abnormality, or a sudden change in pressure. In rare situations, it can occur without any apparent cause.
Patients with a perilymphatic fistula usually complain of a sudden onset of vertigo or dizziness. In more than 50% of patients, a complete loss of hearing also occurs. The diagnosis can only be confirmed at surgery when the hole is actually seen. Although most perilymphatic fistulas will heal spontaneously with rest, in some situations, surgery is performed to patch the hole.
Medication damage to inner ear (ototoxicity)
Ototoxicity refers to the damage caused to the inner ear (labyrinth) from the use of various medications. These medications can damage the inner ear's balance (vestibular) system or hearing (auditory) system or both. It turns out that patients are often bedridden and very ill when given these medications. Therefore, it is often only after they have recovered from their illness that they begin to realize the devastating effects of this damage to the inner ear.
The aminoglycosides are common antibiotics that are known to damage the inner ear. Streptomycin and gentamicin more selectively damage the vestibular system, whereas kanamycin, tobramycin, and amikacin (Amikin) more selectively damage the auditory system. For example, gentamicin toxicity can cause symptoms of imbalance and even oscillopsia. Oscillopsia results from a loss of balance function in both inner ears. As a result, these patients are unable to focus on an object when they move their head or are walking.
Salicylates (e.g., aspirin) can cause hearing loss, ringing in the ears (tinnitus), dizziness, loss of balance, and sometimes vertigo. Unlike other medications that damage the inner ear, however, salicylates cause symptoms of ototoxicity that go away (are reversible) within 24 hours after stopping the drug.
Cisplatinum is a common chemotherapeutic drug used in the treatment of cancer. Unfortunately, it has both auditory and vestibular ototoxicity. The frequency of damage to the inner ear has been reported to be as high as 50% of patients. Its damaging effects can be diminished, however, by a slow administration of the drug and dividing up the dose of the drug over a prolonged time.
Once ototoxicity occurs, the damage is usually irreversible. Physical therapy (vestibular rehabilitation exercises) is often helpful. But, many elderly people lack the ability to fully compensate for the vestibular loss. The key to management of ototoxicity is both patient and physician awareness and prevention of the potential side effects of these drugs. If a patient notices a loss of hearing or a sense of imbalance, these symptoms should be reported to the physician immediately. And, if practical, the drug should be discontinued.
Acoustic neuromas and other cerebellopontine angle (CPA) tumors
An acoustic neuroma is a benign tumor of the insulating cells (Schwann cells) of the eighth cranial (vestibulocochlear) nerve. The tumor develops on the vestibular portion of the eighth cranial nerve as it exits the brainstem at the cerebellopontine angle (CPA). So, the main initial symptoms of an acoustic neuroma are usually related to impaired balance.
An acoustic neuroma is also known as a vestibular schwannoma or a CPA tumor. (Actually, any tumor arising in this location of the brainstem is also known as a CPA tumor.) The vestibular nerve then travels through the internal auditory canal of the temporal bone to the inner ear. In addition to two vestibular branches, the internal auditory canal also houses the single cochlear (hearing) nerve (the other part of the eighth cranial nerve) and the seventh cranial (facial) nerve.
Acoustic neuromas are found sporadically in the population, or specifically in association with a condition called neurofibromatosis Type 2. Neurofibromatosis is a rare inherited disorder associated with bilateral acoustic neuroma tumors and other neural tumors. In either case, both types of acoustic neuromas are associated with a particular genetic (inherited) abnormality (a defect in the NF-2 gene located on chromosome 22). Acoustic neuromas represent 6% of all brain tumors, but 80% of all CPA tumors. Acoustic neuromas occur with an annual incidence of 1 per 100,000 people.
Acoustic neuromas usually grow out from the internal auditory canal spilling into the cerebellopontine angle. As the tumor grows, it compresses and damages the cochlear (hearing) division of the eighth cranial nerve and its blood supply. This nerve damage then results in impaired hearing. For the most part, acoustic neuromas are slow growing. Thus, 90% of these tumors grow at a rate no faster than one mm per year.
Benign paroxysmal positional vertigo (cupulolithiasis)
Benign paroxysmal positional vertigo (BPPV) is a common cause of vertigo. It is characterized by severe episodes of vertigo associated with specific head movement. Notably absent in BPPV are hearing loss, ringing of the ears (tinnitus), and ear fullness. Patients often will describe vertigo after rolling over in bed (usually to only one side) that often will awaken them from sleep. Attacks will also occur after getting up from a bending position, tilting the head back to shave the face or wash the hair, or reaching above the head to take something from a high shelf. Vertigo usually occurs after a 1-2 second delay following the provocative head movement. The vertigo is of short duration, often less than 30 seconds. But many patients will describe a vague type of balance problem (disequilibrium) between episodes.
BPPV increases with advancing age with an annual incidence of 10-50 cases per 100,000 population. There is a slight female predominance. The condition often is associated with head trauma. BPPV is diagnosed clinically based on the typical physical findings of positional vertigo and corresponding involuntary, rapid, repetitive eye movements (nystagmus).
Dislodged tiny stones (cupulolithiasis) in the inner ear cause BPPV. These stones are calcium carbonate crystals that are normally imbedded in a gelatinous mass called the cupula. The cupula overlies the macula, which is a dense structure in the wall of the two sacs -- the utricle and the saccule -- that make up the vestibule. When the stones become dislodged, they float into the semicircular canals of the inner ear. (See the figure.) In fact, microscopic examinations of the inner ears from patients suffering with BPPV have demonstrated these stones.
In the semicircular canals, the stones move from side to side, thereby stimulating the canal. As a result, the canal signals the brain by way of the ampullary branch of the vestibular nerve that it is measuring rotation. Unfortunately, the other ear, the eyes, and the proprioceptive sensors of the body are in mismatch, and the patient then experiences vertigo. Indeed, surgically cutting across (sectioning) the ampullary nerve will immediately stop the vertigo.
Treatment of BPPV is by physical therapy. Thus, repositioning maneuvers, such as the Epley maneuver, are effective by moving the stones from the semi-circular canals back to the cupula in the vestibule of the inner ear.
Vertebral basilar insufficiency
Vertebral basilar insufficiency occurs when there is narrowing of the arteries that supply the posterior brain (subclavian, vertebral, or basilar arteries). It is usually the result of hardening of the arteries (atherosclerosis), and occurs among patients older than 50 years of age. The narrowed arteries decrease the blood flow and, therefore, the oxygen to the vestibular center in the brain. Since the vestibular system is very sensitive to a lack of oxygen, balance problems are often one of the first symptoms of vertebral basilar insufficiency.
Other signs of decreased oxygen to the brain are also usually present. These signs include visual changes, weakness, and fainting. Patients tend to describe their imbalance as lightheadedness that frequently occurs when they stand up quickly. In fact, patients rarely get lightheaded or dizzy when laying flat or resting in a chair. Measuring a drop in blood pressure and an increase in pulse rate when a patient stands upright can confirm the vertebral basilar insufficiency. Other causes of this type of dizziness include heart problems and medication side effects.
Labyrinthitis
Labyrinthitis is an inflammation of the bony or membranous inner ear (labyrinth). Recall that the inner ear is made up of balance (vestibular) and hearing (auditory) components. The bony labyrinth encloses and protects the delicate membranous labyrinth. In general, bacterial infections affect the bony labyrinth and viral infections affect the membranous labyrinth.
Bacterial labyrinthitis: There are three types of bacterial infections that can lead to labyrinthitis: toxic labyrinthitis, acute suppurative (pus-containing) labyrinthitis, and syphilitic labyrinthitis.
In toxic labyrinthitis, bacterial toxins from the middle ear invade the inner ear by passing (diffusing) through the round window of the inner ear. (See the figure.) Both hearing loss and imbalance can occur. Treatment includes antibiotics directed at the bacteria, incision of the eardrum, and drainage of the middle ear space.
Suppurative labyrinthitis is relatively uncommon. It is a bacterial infection characterized by the abrupt (acute) onset of vertigo associated with hearing loss. It is frequently the result of chronic middle ear infections that create a hardened mass of debris and cholesterol (cholesteatoma). The hard mass wears away (erodes) the dense surrounding bone of the inner ear, thereby exposing the inner ear to the infection. The other source of suppurative labyrinthitis is from inflammation of the covering (meninges) of the brain (meningitis).
Syphilitic labyrinthitis is also a bacterial infection of the inner ear. It can be either present at birth (congenital) or acquired. The symptoms are usually fluctuating and slow to develop. But there is a relentless progression to profound or total loss of hearing and balance. A sudden (acute) episode of deafness or dizziness, however, may occur.
The congenital form of syphilitic labyrinthitis may have its onset of symptoms anywhere from birth to age 70. The peak occurrence is between age 30 and 50. Other signs of congenital syphilis are often also present, such as chronic (long duration) eye inflammation (interstitial keratitis) in 90% of patients, Hutchinson's notched teeth, saddle-shaped nose, and swelling of the forehead (frontal bossing).
Syphilitic labyrinthitis is often confused with Meniere disease. The diagnosis of syphilis is established by finding a positive serum fluorescent treponemal antibody absorption test in a patient with the typical clinical history of fluctuating, progressive hearing loss and vertigo. A serum Venereal Disease Research Laboratory (VDRL) test result is positive in only 75% of cases, making it an unreliable test for syphilitic labyrinthitis. Examination of the cerebrospinal fluid (the fluid that surrounds the brain and spinal cord), however, may show a positive VDRL test or the presence of a particular type of white blood cell (lymphocytes) in the fluid. Treatment is with high dose penicillin and cortisone-type drugs.
Viral labyrinthitis (vestibular neuronitis): Labyrinthitis caused by a viral infection is a common condition. It is usually referred to as vestibular neuronitis, viral labyrinthitis, or viral neurolabyrinthitis. Although a viral cause for this disease has not been proven unequivocally, many well conducted population (epidemiological) and tissue microscoscopy (histopathological) studies support a viral cause. Typically, a gradual onset of vertigo, nausea, and vomiting occurs over several hours. Symptoms reach a peak within 24 hours and then gradually improve over several days. Most patients have complete recovery within 6 weeks. Treatment is directed at suppression of symptoms. This includes vestibular suppressants like diazepam (Valium), vestibular exercises, and hydration. Some evidence suggests that high-dose cortisone-type drugs given early in the disease with or without antiviral agents may be helpful.
Multiple sclerosis
Multiple sclerosis (MS) is a demyelinating (loss of nerve cell insulation) brain disorder of unknown cause. MS usually follows a course of alternating improved symptoms (remissions) and worsening symptoms (exacerbations). Although vertigo or dizziness is not often the only indication of multiple sclerosis, it is a common symptom that occurs at some point in the illness. Thus, vertigo is the initial symptom in about 5% of patients, but is reported at some time during the disease by as many as 50%. In addition, hearing loss occurs in about 10% of patients. The diagnosis of MS is suggested when a young adult has a history of multiple neurological abnormalities (e.g., visual disturbance, muscle weakness, speech impediment, and mental changes) characterized by remissions and exacerbations.
Disequilibrium of aging
As individuals age, there is a general decrease in vestibular function. This decrease is accompanied by a general decrease in vision, position (proprioception) sense, muscle and bone strength, and brain function. All of these changes combined often lead to a slowly progressive feeling of imbalance (disequilibrium). Nevertheless, these changes may be compensated in large part by visual input. Consequently, elderly patients may notice more balance problems at night. A general physical examination is important to rule-out other serious conditions such as tumors or stroke that can cause balance problems.
Finally, a particular set of symptoms -- dizziness, unsteady walking, increased frequency of urination, and forgetfulness -- may occur in elderly patients due to a condition called a communicating hydrocephalus. In this condition, a subtle accumulation of cerebrospinal fluid occurs in the brain due to a failure of absorption of the fluid. There is no obstruction (blockage) of the cerebrospinal fluid and the pressure of the fluid is normal. Nevertheless, creating a shunt for drainage of the excess fluid can improve the symptoms.
Vestibular Balance Disorders at a Glance
- Dizziness is defined as a feeling of being woozy, drunk, unsteady, or giddy. It is a general term used to describe the sensation of imbalance.
- Vertigo refers to an hallucination of motion, and is often described as a spinning sensation. It usually implies a disorder of the inner ear.
- Lightheadedness indicates the sensation that occurs prior to fainting. It is caused by a momentary decrease in blood flow to the brain.
- Motion sickness is a normal response to an abnormal situation when there is conflicting information going to the brain from the eyes and the inner ear.
- Diseases that affect the eyes, ears, general sensory system (skin, muscle, and joints), and the brain can cause balance problems.
- A patient's description of a balance problem is often the key to the clinical diagnosis. Particularly helpful factors are the duration of the attack and any triggering events.
- Special tests of balance function, hearing tests, CAT scan, and MRI scan are often done to help make the diagnosis of a balance disorder. Referral to an ear specialist or neurologist may be necessary.
- Patients with balance problems need to take proper precautions to avoid accidents that could be caused by their balance disorder.
- Vestibular rehabilitation involves special exercises to help a patient with a balance disorder adjust (accommodate) to the balance problem so as to diminish recurrent symptoms.
- Common conditions causing balance problems include Meniere disease, motion sickness syndrome, vestibular migraines, inner ear trauma, perilymphatic fistula, medication damage to inner ear (ototoxicity), acoustic neuromas and other brain tumors, benign paroxysmal positional vertigo, vertebral basilar insufficiency, bacterial labyrinthitis, viral labyrinthitis (vestibular neuronitis), multiple sclerosis, and disequilibrium of aging.
|
Bookmark this post:
|
|



0 comments
Post a Comment