
What is septic arthritis?
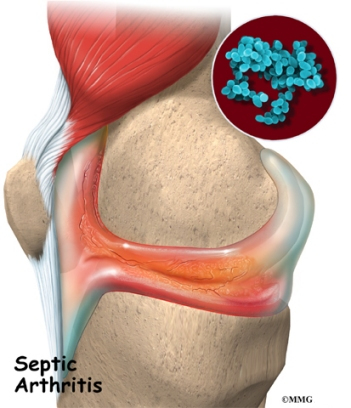
Septic, or infectious, arthritis is infection of one or more joints by microorganisms. Normally, the joint is lubricated with a small amount of fluid that is referred to as synovial fluid or joint fluid. The normal joint fluid is sterile and, if removed and cultured in the laboratory, no microbes will be found. With septic arthritis, microbes are identifiable in an affected joint fluid.
Most commonly, septic arthritis affects a single joint, but occasionally more joints are involved. The joints affected vary somewhat depending on the microbe causing the infection and the predisposing risk factors of the person affected. Septic arthritis is also called infectious arthritis.
What microbes cause septic arthritis?
Septic arthritis can be caused by bacteria, viruses, and fungi. The most common causes of septic arthritis are bacteria, including Staphylococcus aureus and Haemophilus influenzae. In certain "high-risk" individuals, other bacteria may cause septic arthritis, such as E. coli and Pseudomonas spp. in intravenous drug abusers and the elderly, Neisseria gonorrhoeae in sexually active young adults, and Salmonella spp. in young children or in people with sickle cell disease. Other bacteria that can cause septic arthritis include Mycobacterium tuberculosis and the spirochete bacterium that causes Lyme disease.
Viruses that can cause septic arthritis include hepatitis A, B, and C, parvovirus B19, herpes viruses, HIV (AIDS virus), HTLV-1, adenovirus, coxsackie viruses, mumps, and ebola. Fungi that can cause septic arthritis include histoplasma, coccidiomyces, and blastomyces.
Who is at risk of developing septic arthritis?
While joint infection occasionally affects people with no known predisposing risk factors, it more commonly occurs when certain risk situations are present. Risks for the development of septic arthritis include taking medications that suppress the immune system, intravenous drug abuse, past joint disease, injury, or surgery, and underlying medical illnesses including diabetes, alcoholism, sickle cell disease, rheumatic diseases, and immune deficiency disorders. People with any of these conditions who develop symptoms of septic arthritis should promptly seek medical attention.
What are symptoms and signs of septic arthritis?
Symptoms of septic arthritis include fever, chills, as well as joint pain, swelling, redness, stiffness, and warmth. Joints most commonly involved are large joints, such as the knees, ankles, hips, and elbows. In people with risk factors for joint infection, unusual joints can be infected, including the joint where the collar bone (clavicle) meets the breastbone (sternum). With uncommon microbes, such as Brucella spp., atypical joints can be infected, such as the sacroiliac joints.
How is septic arthritis diagnosed?
Septic arthritis is diagnosed by identifying infected joint fluid. Joint fluid can easily be removed sterilely in the office, clinic, or hospital with a needle and syringe. The fluid is analyzed in a laboratory to determine if there is an elevated number of white blood cells to suggest inflammation. A culture of the joint fluid can identify the particular microbe and determine its susceptibility to a variety of antibiotics.
X-ray studies of the joint can be helpful to detect injury of bone adjacent to the joint. MRI scanning is very sensitive in evaluating joint destruction. Blood tests are frequently used to detect and monitor inflammation. These tests include the white blood cell count, sedimentation rate, and C-reactive protein.
How is septic arthritis treated?
Septic arthritis is treated with antibiotics and drainage of the infected joint (synovial) fluid from the joint.
Optimally, antibiotics are given immediately. Often, intravenous antibiotics are administered in a hospital setting. The choice of antibiotics can be guided by the results of the culture of joint fluid. Until those results are known, empiric antibiotics are chosen to cover a wider range of possible infectious agents. Sometimes, combinations of antibiotics are given. Antibiotics can be required for four to six weeks.
Drainage is essential for rapid clearing of the infection. Drainage can be done by regular aspirations with a needle and syringe, often daily early on, or via surgical procedures. Arthroscopy can be used to irrigate the joint and remove infected joint lining tissue. If adequate drainage cannot be accomplished with joint aspirations or arthroscopy, open joint surgery is used to drain the joint. After arthroscopy or open joint surgery, drains are sometimes left in place to drain excess fluid that can accumulate after the procedure.

What are complications of septic arthritis?
Rapid clearing of the infection is critical to preserve the joint. If appropriate antibiotics are begun immediately, joint integrity can be maintained, and return to function is expected. If the infection has been long-standing, the possibility of joint destruction exists. The keys to successful outcome are rapid medical attention and drainage and the accurate administration of antibiotics to which the offending microbes are susceptible.
Septic Arthritis At A Glance
- Septic arthritis is infection of one or more joints by microorganisms.
- Septic arthritis can be caused by bacteria, viruses, and fungi.
- Risks for the development of septic arthritis include taking immune-suppression medicines, intravenous drug abuse, past joint disease, injury or surgery, and underlying medical illnesses including diabetes, alcoholism, sickle cell disease, rheumatic diseases, and immune deficiency disorders.
- Symptoms of septic arthritis include fever, chills, as well as joint pain, swelling, redness, stiffness, and warmth.
- Septic arthritis is diagnosed by identifying infected joint fluid.
- Septic arthritis is treated with antibiotics and drainage of the infected joint fluid from the joint.
|
Bookmark this post:
|
|

0 comments
Post a Comment