
Introduction
Skin cancer is the most common form of human cancer. It is estimated that over 1 million new cases occur annually. The annual rates of all forms of skin cancer are increasing each year, representing a growing public concern. It has also been estimated that nearly half of all Americans who live to age 65 will develop skin cancer at least once.
The most common warning sign of skin cancer is a change in the appearance of the skin, such as a new growth or a sore that will not heal.
The term "skin cancer" refers to three different conditions. From the least to the most dangerous, they are:
- basal cell carcinoma (or basal cell carcinoma epithelioma)
- squamous cell carcinoma (the first stage of which is called actinic keratosis)
- melanoma
The two most common forms of skin cancer are basal cell carcinoma and squamous cell carcinoma. Together, these two are also referred to as nonmelanoma skin cancer. Melanoma is generally the most serious form of skin cancer because it tends to spread (metastasize) throughout the body quickly. Skin cancer is also known as skin neoplasia.
This article will discuss the two kinds of nonmelanoma skin cancer.
Basal cell carcinoma
What is basal cell carcinoma?
Basal cell carcinoma is the most common form of skin cancer and accounts for more than 90% of all skin cancer in the U.S. These cancers almost never spread (metastasize) to other parts of the body. They can, however, cause damage by growing and invading surrounding tissue.
What are risk factors for developing basal cell carcinoma?
Light-colored skin, sun exposure, and age are all important factors in the development of basal cell carcinomas. People who have fair skin and are older have higher rates of basal cell carcinoma. About 20% of these skin cancers, however, occur in areas that are not sun-exposed, such as the chest, back, arms, legs, and scalp. The face, however, remains the most common location for basal cell lesions. Weakening of the immune system, whether by disease or medication, can also promote the risk of developing basal cell carcinoma. Other risk factors include
- exposure to sun. There is evidence that, in contrast to squamous cell carcinoma, basal cell carcinoma is promoted not by accumulated sun exposure but by intermittent sun exposure like that received during vacations, especially early in life. According to the U.S. National Institutes of Health, ultraviolet (UV) radiation from the sun is the main cause of skin cancer. The risk of developing skin cancer is also affected by where a person lives. People who live in areas that receive high levels of UV radiation from the sun are more likely to develop skin cancer. In the United States, for example, skin cancer is more common in Texas than it is in Minnesota, where the sun is not as strong. Worldwide, the highest rates of skin cancer are found in South Africa and Australia, which are areas that receive high amounts of UV radiation.
- age. Most skin cancers appear after age 50, but the sun's damaging effects begin at an early age. Therefore, protection should start in childhood in order to prevent skin cancer later in life.
- exposure to ultraviolet radiation in tanning booths. Tanning booths are very popular, especially among adolescents, and they even let people who live in cold climates radiate their skin year-round.
- therapeutic radiation, such as that given for treating other forms of cancer.
What does basal cell carcinoma look like?

A basal cell carcinoma usually begins as a small, dome-shaped bump and is often covered by small, superficial blood vessels called telangiectases. The texture of such a spot is often shiny and translucent, sometimes referred to as "pearly." It is often hard to tell a basal cell carcinoma from a benign growth like a flesh-colored mole without performing a biopsy. Some basal cell carcinomas contain melanin pigment, making them look dark rather than shiny.
Superficial basal cell carcinomas often appear on the chest or back and look more like patches of raw, dry skin. They grow slowly over the course of months or years.
Basal cell carcinomas grow slowly, taking months or even years to become sizable. Although spread to other parts of the body (metastasis) is very rare, a basal cell carcinoma can damage and disfigure the eye, ear, or nose if it grows nearby.
How is basal cell carcinoma diagnosed?
To make a proper diagnosis, doctors usually remove all or part of the growth by performing a biopsy. This usually involves taking a sample by injecting a local anesthesia and scraping a small piece of skin. This method is referred to as a shave biopsy. The skin that is removed is then examined under a microscope to check for cancer cells.
How is basal cell carcinoma treated?
There are many ways to successfully treat a basal cell carcinoma with a good chance of success of 90% or more. The doctor's main goal is to remove or destroy the cancer completely with as small a scar as possible. To plan the best treatment for each patient, the doctor considers the location and size of the cancer, the risk of scarring, and the person's age, general health, and medical history.
Methods used to treat basal cell carcinomas include:
- Curettage and desiccation: Dermatologists often prefer this method, which consists of scooping out the basal cell carcinoma by using a spoon like instrument called a curette. Desiccation is the additional application of an electric current to control bleeding and kill the remaining cancer cells. The skin heals without stitching. This technique is best suited for small cancers in non-crucial areas such as the trunk and extremities.
- Surgical excision: The tumor is cut out and stitched up.
- Radiation therapy: Doctors often use radiation treatments for skin cancer occurring in areas that are difficult to treat with surgery. Obtaining a good cosmetic result generally involves many treatment sessions, perhaps 25 to 30.
- Cryosurgery: Some doctors trained in this technique achieve good results by freezing basal cell carcinomas. Typically, liquid nitrogen is applied to the growth to freeze and kill the abnormal cells.
- Mohs micrographic surgery: Named for its pioneer, Dr. Frederic Mohs, this technique of removing skin cancer is better termed "microscopically controlled excision." The surgeon meticulously removes a small piece of the tumor and examines it under the microscope during surgery. This sequence of cutting and microscopic examination is repeated in a painstaking fashion so that the basal cell carcinoma can be mapped and taken out without having to estimate or guess the width and depth of the lesion. This method removes as little of the healthy normal tissue as possible. Cure rate is very high, exceeding 98%. Mohs micrographic surgery is preferred for large basal cell carcinomas, those that recur after previous treatment, or lesions affecting parts of the body where experience shows that recurrence is common after treatment by other methods. Such body parts include the scalp, forehead, ears, and the corners of the nose. In cases where large amounts of tissue need to be removed, the Mohs surgeon sometimes works with a plastic (reconstructive) surgeon to achieve the best possible postsurgical appearance.
- Medical therapy using creams that attack cancer cells (5-Fluorouracil--5-FU, Efudex, Fluoroplex) or stimulate the immune system (imiquimod [Aldara]). These are applied several times a week for several weeks. They produce brisk inflammation and irritation. The advantages of this method is that it avoids surgery, lets the patient perform treatment at home, and may give a better cosmetic result. Disadvantages include discomfort, which may be severe, and a lower cure rate, which makes medical treatment unsuitable for treating most skin cancers on the face.
How is basal cell carcinoma prevented?
Avoiding sun exposure in susceptible individuals is the best way to lower the risk for all types of skin cancer. Regular surveillance of susceptible individuals, both by self-examination and regular physical examination, is also a good idea for people at higher risk. People who have already had any form of skin cancer should have regular medical checkups.
Common sense preventive techniques include
- limiting recreational sun exposure;
- avoiding unprotected exposure to the sun during peak radiation times (the hours surrounding noon);
- wearing broad-brimmed hats and tightly-woven protective clothing while outdoors in the sun;
- regularly using a waterproof or water resistant sunscreen with UVA protection and SPF 30 or higher;
- undergoing regular checkups and bringing any suspicious-looking or changing lesions to the attention of the doctor; and
- avoiding the use of tanning beds and using a sunscreen with an SPF of 30 and protection against UVA (long waves of ultraviolet light.). Many people go out of their way to get an artificial tan before they leave for a sunny vacation, because they want to get a "base coat" to prevent sun damage. Even those who are capable of getting a tan, however, only get protection to the level of SPF 6, whereas the desired level is an SPF of 30. Those who only freckle get little or no protection at all from attempting to tan; they just increase sun damage. Sunscreen must be applied liberally and reapplied every two to three hours, especially after swimming or physical activity that promotes perspiration, which can weaken even sunscreens labeled as "waterproof."
Squamous cell carcinoma
What is squamous cell carcinoma?
Squamous cell carcinoma is cancer that begins in the squamous cells, which are thin, flat cells that look like fish scales under the microscope. The word squamous came from the Latin squama, meaning "the scale of a fish or serpent" because of the appearance of the cells.
Squamous cells are found in the tissue that forms the surface of the skin, the lining of the hollow organs of the body, and the passages of the respiratory and digestive tracts. Thus, squamous cell carcinomas can actually arise in any of these tissues.
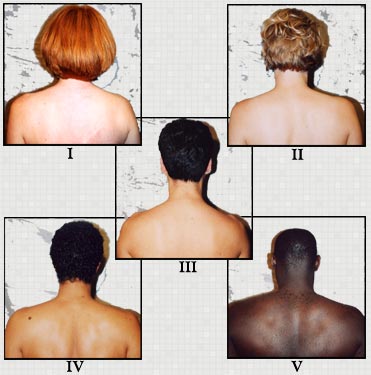
Squamous cell carcinoma of the skin occurs roughly one-quarter as often as basal cell carcinoma. Light-colored skin and a history of sun exposure are even more important in predisposing to this kind of cancer than to basal cell carcinoma. Men are affected more often than women. Patterns of dress and hairstyle may play a role. Women, whose hair generally covers their ears, develop squamous cell carcinomas far less often in this location than do men.
The earliest form of squamous cell carcinoma is called actinic (or solar) keratosis. Actinic keratoses appear as rough, red bumps on the scalp, face, ears, and backs of the hands. They often appear against a background of mottled, sun-damaged skin. They can be quite sore and tender, out of proportion to their appearance. In a patient with actinic keratoses, the rate at which one such keratosis may invade deeper in the skin to become a fully-developed squamous cell carcinoma is estimated to be in the range of 10%-20% over 10 years, though it may take less time. An actinic keratosis that becomes thicker and more tender raises the concern that it may have transformed into an invasive squamous cell carcinoma.
A rapidly-growing form of squamous cell carcinoma that forms a mound with a central crater is called a keratoacanthoma. While some consider this not a true cancer but instead a condition that takes care of itself, most pathologists consider it to be a form of squamous cell cancer and clinicians treat is accordingly.
Other forms of squamous cell carcinoma that have not yet invaded deeper into the skin include
- actinic cheilitis, involving the lower lip with redness and scale, and blurring the border between the lip and the surrounding skin;
- Bowen's disease, sometimes referred to as squamous cell carcinoma in situ. (The Latin words in situ refer to the presence of the cancer only in the superficial epidermis, without deeper involvement.) Bowen's disease appears as scaly patches on sun-exposed parts of the trunk and extremities; and
- Bowenoid papulosis: These are genital warts that under the microscope look like Bowen's disease but behave like warts, not like cancers.
What are risk factors for developing squamous cell carcinoma?
The single most important factor in producing squamous cell carcinomas is sun exposure. Many such growths can develop from precancerous spots, called actinic or solar keratoses. These lesions appear after years of sun damage on parts of the body like the forehead and cheeks, as well as the backs of the hands. Sun damage takes many years to promote skin cancer. It is therefore common for people who stopped being "sun worshipers" in their 20s to develop precancerous or cancerous spots decades later.
Several rather uncommon factors may predispose to squamous cell carcinoma. These include exposure to arsenic, hydrocarbons, heat, or X-rays. Some squamous cell carcinomas arise in scar tissue. Suppression of the immune system by infection or drugs may also promote such growths. Some strains of HPV (the human papillomavirus responsible for causing genital warts) can promote development of squamous cell carcinoma in the anogenital region.
Can squamous cell carcinoma of the skin spread (metastasize)?
Yes. Unlike basal cell carcinomas, squamous cell carcinomas can metastasize, or spread to other parts of the body. These tumors usually begin as firm, skin-colored or red nodules. Squamous cell cancers that start out within solar keratoses or on sun-damaged skin are easier to cure and metastasize less often than those that develop in traumatic or radiation scars. One location particularly prone to metastatic spread is the lower lip. A proper diagnosis in this location is, therefore, especially important.
How is squamous cell carcinoma diagnosed?
As with basal cell carcinoma, doctors usually perform a biopsy to make a proper diagnosis. This involves taking a sample by injecting local anesthesia and punching out a small piece of skin using a circular punch blade. Usually the method used referred to as a punch biopsy. The skin that is removed is then examined under a microscope to check for cancer cells.
How is squamous cell carcinoma treated?
Techniques for treating squamous cell carcinoma are similar to those for basal cell carcinoma (for detailed descriptions, see above under treatment of basal cell carcinoma):
- Curettage and desiccation: Dermatologists often prefer this method, which consists of scooping out the basal cell carcinoma by using a spoon like instrument called a curette. Desiccation is the additional application of an electric current to control bleeding and kill the remaining cancer cells. The skin heals without stitching. This technique is best suited for small cancers in non-crucial areas such as the trunk and extremities.
- Surgical excision: The tumor is cut out and stitched up.
- Radiation therapy: Doctors often use radiation treatments for skin cancer occurring in areas that are difficult to treat with surgery. Obtaining a good cosmetic result generally involves many treatment sessions, perhaps 25 to 30.
- Cryosurgery: Some doctors trained in this technique achieve good results by freezing basal cell carcinomas. Typically, liquid nitrogen is applied to the growth to freeze and kill the abnormal cells.
- Mohs micrographic surgery: Named for its pioneer, Dr. Frederic Mohs, this technique of removing skin cancer is better termed, "microscopically controlled excision." The surgeon meticulously removes a small piece of the tumor and examines it under the microscope during surgery. This sequence of cutting and microscopic examination is repeated in a painstaking fashion so that the basal cell carcinoma can be mapped and taken out without having to estimate or guess the width and depth of the lesion. This method removes as little of the healthy normal tissue as possible. Cure rate is very high, exceeding 98%. Mohs micrographic surgery is preferred for large basal cell carcinomas, those that recur after previous treatment, or lesions affecting parts of the body where experience shows that recurrence is common after treatment by other methods. Such body parts include the scalp, forehead, ears, and the corners of the nose. In cases where large amounts of tissue need to be removed, the Mohs surgeon sometimes works with a plastic (reconstructive) surgeon to achieve the best possible postsurgical appearance.
- Medical therapy using creams that attack cancer cells (5-Fluorouracil--5-FU, Efudex, Fluoroplex) or stimulate the immune system (Aldara). These are applied several times a week for several weeks. They produce brisk inflammation and irritation. The advantages of this method is that it avoids surgery, lets the patient perform treatment at home, and may give a better cosmetic result. Disadvantages include discomfort, which may be severe, and a lower cure rate, which makes medical treatment unsuitable for treating most skin cancers on the face.
The possibility of metastasis makes it especially important to diagnose squamous cell carcinomas early and treat them adequately.
How is squamous cell carcinoma prevented?
Even more so than is the case with basal cell carcinoma, the key principles of prevention are minimizing sun exposure and getting regular checkups.
Common-sense preventive techniques are the same as for basal cell carcinoma and include
- limiting recreational sun exposure;
- avoiding unprotected exposure to the sun during peak radiation times (the hours surrounding noon);
- wearing broad-brimmed hats and tightly-woven protective clothing while outdoors in the sun;
- regularly using a waterproof or water-resistant sunscreen with UVA protection and SPF 30 or higher;
- undergoing regular checkups and bringing any suspicious-looking or changing lesions to the attention of a doctor; and
- avoiding the use of tanning beds and using a sunscreen with an SPF 30 and protection against UVA (long waves of ultraviolet light). Many people go out of their way to get an artificial tan before they leave for a sunny vacation, because they want to get a "base coat" to prevent sun damage. Even those who are capable of getting a tan, however, only get protection to the level of SPF 6, whereas the desired level is an SPF of 30. Those who only freckle get little or no protection at all from attempting to tan; they just increase sun damage. Sunscreen must be applied liberally and reapplied every two to three hours, especially after swimming or physical activity that promotes perspiration, which can weaken even sunscreens labeled as "waterproof."
What about follow-up care for skin cancer?
Skin cancer has a better prognosis, or outcome, than most other types of cancer. It is generally curable. Even though most skin cancers are cured, people who have been treated for skin cancer have a higher-than-average risk of developing a new cancer of the skin. This is the reason why it is so important for patients to continue to examine themselves regularly, visit their doctor for regular checkups, and follow their doctor's instructions on how to reduce their risk of developing skin cancer again.
How about vitamin D and cancer?
Some recent reports suggest that getting vitamin D from sun exposure may prevent the occurrence and spread of cancers, both of internal organs and of the skin. In spite of the occasional controversy surrounding these studies, their common-sense implications are simple enough. Even those doctors who recommend sun for vitamin D only suggest 15 minutes a few times a week. For most people, especially those who have day jobs or live in cooler climates, following this advice is not likely to result in markedly higher risk of skin cancer. No responsible authority suggests that to help with vitamin D, people ought to sunbathe or visit tanning salons.
What resources are available to patients with skin cancer?
Skin Cancer Foundation
245 Fifth Avenue, Suite 2402
New York, NY 10016
212-725-5176
This nonprofit organization provides publications and audiovisual materials on the prevention, early detection, and treatment of skin cancer. The foundation also publishes Sun and Skin News and The Skin Cancer Foundation Journal, which have nontechnical articles on skin cancer. Send a stamped, self-addressed envelope to the above address to receive free printed information.
American Academy of Dermatology
PO Box 4014
Schaumburg, IL 60168-4014
708-330-0230
The American Academy of Dermatology is an organization of doctors who specialize in diagnosing and treating skin problems. It provides free booklets on skin cancer and can refer people to dermatologists in their local area.
American Society of Plastic and Reconstructive Surgeons
444 East Algonquin Road
Arlington Heights, IL 60005
1-800-635-0635
This society sends free information about various surgical procedures. It can also provide the names of board-certified plastic surgeons in a patient's area.
Skin Cancer At A Glance
- There are three main types of skin cancer: basal cell carcinoma, squamous cell carcinoma (the nonmelanoma skin cancers), and melanoma.
- Skin cancer is the most common form of cancer in humans.
- Ultraviolet light, which is in sunlight, is the main cause of skin cancer.
- The most common warning sign of skin cancer is a change in the appearance of the skin, such as a new growth or a sore that will not heal. Unexplained changes in the appearance of the skin lasting longer than two weeks should be evaluated by a doctor.
- Nonmelanoma skin cancer is generally curable. The cure rate for nonmelanoma skin cancer could be 100% if these lesions were brought to a doctor's attention before they had a chance to spread.
- Treatment of nonmelanoma skin cancer depends on the type and location of the skin cancer, the risk of scarring, as well as the age and health of the patient. Methods used include curettage and desiccation, surgical excision, cryosurgery, radiation, and Mohs micrographic surgery.
- Avoiding sun exposure in susceptible individuals is the best way to lower the risk for all types of skin cancer. Regular surveillance of susceptible individuals, both by self-examination and regular physical examination, is also a good idea for people at higher risk. People who have already had any form of skin cancer should have regular medical checkups.
sourceLast Editorial Review: 4/9/2008
|
Bookmark this post:
|
|




0 comments
Post a Comment