What is high blood pressure?
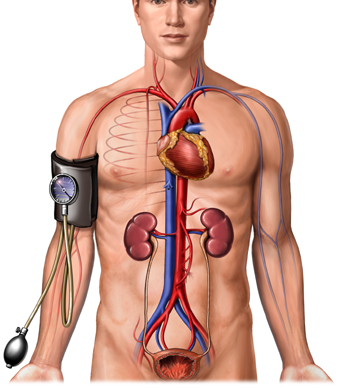
High blood pressure or hypertension means high pressure (tension) in the arteries. Arteries are vessels that carry blood from the pumping heart to all the tissues and organs of the body. High blood pressure does not mean excessive emotional tension, although emotional tension and stress can temporarily increase blood pressure. Normal blood pressure is below 120/80; blood pressure between 120/80 and 139/89 is called "pre-hypertension", and a blood pressure of 140/90 or above is considered high.
The top number, which is the systolic blood pressure, corresponds to the pressure in the arteries as the heart contracts and pumps blood into the arteries. The bottom number, the diastolic pressure, represents the pressure in the arteries as the heart relaxes after the contraction. The diastolic pressure reflects the lowest pressure to which the arteries are exposed.
An elevation of the systolic and/or diastolic blood pressure increases the risk of developing heart (cardiac) disease, kidney (renal) disease, hardening of the arteries (atherosclerosis or arteriosclerosis), eye damage, and stroke (brain damage). These complications of hypertension are often referred to as end-organ damage because damage to these organs is the end result of chronic (long duration) high blood pressure. For that reason, the diagnosis of high blood pressure is important so efforts can be made to normalize blood pressure and prevent complications.
It was previously thought that rises in diastolic blood pressure were a more important risk factor than systolic elevations, but it is now known that in people 50 years and older systolic hypertension represents a greater risk.
Affecting approximately one in four adults in the United States, hypertension is clearly a major public health problem.
Which lifestyle modifications are beneficial in treating high blood pressure?
Lifestyle modifications refer to certain specific recommendations for changes in habits, diet and exercise. These modifications can lower the blood pressure as well as improve a patient's response to blood pressure medications.
Alcohol
People who drink alcohol excessively (over two drinks per day) have a one and a half to two times increase in the prevalence of hypertension. The association between alcohol and high blood pressure is particularly noticeable when alcohol intake exceeds five drinks per day. The connection is a dose-related phenomenon. In other words, the more alcohol consumed, the stronger is the link with hypertension.
Smoking
Although smoking increases the risk of vascular complications (for example, heart disease and stroke) in people who already have hypertension, it is not associated with an increase in the development of hypertension. But cigarette smoking can repeatedly produce an immediate, temporary rise in the blood pressure of 5 to10 mm Hg. Steady smokers however, may have a lower blood pressure than nonsmokers. The reason for this is that nicotine in cigarettes causes a decrease in appetite, which leads to weight loss. This, in turn, lowers blood pressure.
Coffee
In one study, the caffeine consumed in 5 cups of coffee daily caused a mild increase in blood pressure in elderly people who already had hypertension, but not in those who had normal blood pressures. What's more, the combination of smoking and drinking coffee in persons with high blood pressure may increase the blood pressure more than coffee alone. Limiting caffeine intake and cigarette smoking in hypertensive individuals may be of some benefit in controlling high blood pressure.
Salt
The American Heart Association recommends consumption of dietary salt be less than 6 grams of salt per day in the general population and a lower level (less than 4 grams) for people with hypertension. To achieve a diet containing less than 4 grams of salt, do not add salt to food or cooking. Also, the amount of natural salt in the diet can be reasonably estimated from the labeling information provided with most purchased foods. Note: Take care if using salt substitutes, as some contain sodium!
Other dietary considerations
Add potassium to your diet. Studies show that people who consume more potassium have lower blood pressures. Good sources of potassium include:
- bananas,
- melons,
- oranges,
- spinach and
- zucchini.
Check with your doctor first if you are being treated for kidney failure as potassium rich foods may be harmful to you.
The DASH Diet (Dietary Approaches to Stop Hypertension) was established by the National Heart, Lung and Blood Institute NHLBI. It emphasizes whole grains, fruits and vegetables, low-fat dairy and meats.
Some supplements, such as garlic and flax seed have been shown in studies to lower blood pressure. Garlic may react with some prescription medications such as blood thinners, so consult your physician before taking any supplements.
Obesity
Obesity is common among hypertensive patients, and its prevalence, especially in aging patients, can contribute to hypertension in several ways. In obese people the heart has to pump out more blood to supply the excess tissue. The increased cardiac output then can raise the blood pressure. In addition, obese hypertensive individuals have a greater stiffness (resistance) in their peripheral arteries throughout the body. Insulin resistance and the metabolic syndrome also occur more frequently in the obese. Finally, obesity may be associated with a tendency for the kidneys to retain salt. Weight loss may help reverse obesity-related problems and may lower blood pressure. Blood pressure may be decreased 0.32 mm Hg for every 1 kg (2.2 pounds) of weight lost down to a person's ideal body weight.
Some very obese people have a syndrome called sleep apnea, characterized by periodic interruption of normal breathing during sleep. sleep apnea may contribute to the development of hypertension in this subgroup of obese individuals. Repeated episodes of apnea cause a lack of oxygen (hypoxia), causing the adrenal gland to release adrenaline and related substances which cause a rise in the blood pressure.
Exercise
A regular exercise program may help lower blood pressure over the long term. Activities such as jogging, bicycle riding, power walking, or swimming for 30 to 45 minutes daily may lower blood pressure by as much as 5 to15 mm Hg. There also appears to be a relationship between the amount of exercise and the degree to which the blood pressure is lowered. So the more you exercise (up to a point), the more you lower the blood pressure. This beneficial response occurs only with aerobic (vigorous and sustained) exercise programs. Any exercise program must be recommended or approved by a physician.
How is high blood pressure treated?
Goals of treatment
Keep in mind that high blood pressure is usually present for many years before its complications develop. Ideally, hypertension is treated early, before it damages critical organs in the body. Increased public awareness and screening programs to detect early, uncomplicated hypertension are keys to successful treatment. By treating high blood pressure successfully early enough, you can significantly decrease the risk of stroke, heart attack, and kidney failure.
The goal for patients with combined systolic and diastolic hypertension is to attain a blood pressure of 140/85 mm Hg. Bringing the blood pressure down even lower may be desirable in African American patients, and patients with diabetes or chronic kidney disease. Although life style changes in pre-hypertensive patients are appropriate, it is not well established that treatment with medication of patients with pre-hypertension is beneficial.
Starting treatment for high blood pressure
Blood pressure persistently higher than 140/ 90 mm Hg usually is treated with lifestyle modifications and medication. More aggressive treatment may be recommended in certain circumstances if the diastolic pressure remains at a borderline level (usually less than 90 mm Hg, yet persistently above 85). These circumstances include borderline diastolic pressures in association with end-organ damage, systolic hypertension, or factors that increase the risk of cardiovascular disease, such as age over 65 years, African American decent, smoking, hyperlipemia (elevated blood fats), or diabetes.
Any one of the several classes of medications may be started, except the alpha-blocker medications. The alpha-blockers are used only in combination with another anti-hypertensive medication in specific medical situations. (See the next section for a more detailed discussion of each of the several classes of anti-hypertensive medications.)
In some situations, certain classes of anti-hypertensive drugs are preferable to others as the first line (preferred first choice) drugs. Angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blocking (ARB) drugs are the drugs of choice in patients with heart failure, chronic kidney failure (in diabetics or non-diabetics), or heart attack (myocardial infarction) that weakens the heart muscle (systolic dysfunction). Also, beta-blockers are sometimes the preferred treatment in hypertensive patients with a resting tachycardia (racing heart beat when resting) or an acute (rapid onset, current) heart attack.
Patients with hypertension may sometimes have a co-existing, second medical condition. In such cases, a particular class of anti-hypertensive medication or combination of drugs may be chosen as the first line approach. The idea in these cases is to control the hypertension while also benefiting the second condition. For example, beta-blockers may treat chronic anxiety or migraine headache as well as hypertension. Also, the combination of an ACE inhibitor and an ARB drug can be used to treat certain diseases of the heart muscle (cardiomyopathies) and certain kidney diseases where reduction in proteinuria would be beneficial.
In other situations, certain classes of anti-hypertensive medications should not be used (are contraindicated). Dihydropyridine calcium channel blockers used alone may cause problems for patients with chronic renal disease by increasing proteinuria. However, an ACE inhibitor will blunt this effect. The non-dihydropyridine type of calcium channel blockers should not be used in patients with heart failure. However, these drugs may be beneficial in treating certain arrhythmias. Some drugs, such as minoxidil, since it is so powerful, usually are relegated to second or third line choices for treatment. Clonidine is an excellent drug but has side effects such as fatigue, sleepiness, and dry month making it a second or third line choice. See the section below on pregnancy for the anti-hypertensive drugs that are appropriate or inappropriate for use in pregnant women.
Treatment with combinations of drugs for high blood pressure
The use of combination drug therapy for hypertension is common. At times, using smaller amounts of one or more drugs in combination can minimize side effects while maximizing the anti-hypertensive effect. For example, diuretics, which also can be used alone, are more often used in a low dose in combination with another class of anti-hypertensive medications. This way, the diuretic has fewer side effects while improving the blood pressure - lowering effect of the other drug. Diuretics also are added to other anti-hypertensive medications when a patient with hypertension also has fluid retention and swelling (edema).
ACE inhibitors or angiotensin receptor blockers may be useful in combination with most other anti-hypertensive medications. These kinds of drugs have additive effects in treating patients with cardiomyopathies and proteinuria. Another useful combination is that of a beta-blocker with an alpha-blocker in patients with high blood pressure and enlargement of the prostate gland in order to treat both conditions simultaneously. But caution is necessary when combining two drugs that both lower the heart rate. For example, patients receiving a combination of a beta-blocker to a non-dihydropyridine calcium channel blocker [for example, diltiazem (Cardizem, Dilacor, Tiazac) or verapamil (Calan, Verelan, Isoptin, Covera-HS)] need to be monitored carefully to avoid an excessively slow heart rate (bradycardia). Combining alpha and beta-blockers such as carvedilol (Coreg) and labetalol (Normodyne, Trandate) is useful for cardiomyopathies and for hypertension patients.
Emergency treatment of high blood pressure
In a hospital setting, injectable drugs may be used for emergency treatment of hypertension. The most commonly used are sodium nitroprusside (Nipride) and labetalol (Normodyne). Emergency medical therapy is needed for patients with severe (malignant) hypertension and in patients with short duration (acute) congestive heart failure, dissecting aneurysm (dilation or widening) of the aorta, stroke, and toxemia of pregnancy (see below).
Treatment during pregnancy
Pregnant women may develop hypertension or may have it already before conception. These patients have an increased risk of developing preeclampsia or eclampsia (toxemia of pregnancy). These conditions usually develop during the last three months (trimester) of pregnancy. In preeclampsia, which can occur with or without pre-existing hypertension, affected women have hypertension, protein loss in the urine (proteinuria), and swelling (edema). In eclampsia convulsions also occur and the hypertension requires emergency treatment. The baby must be delivered quickly as part of the treatment of the mother. The main goal of treating the high blood pressure in toxemia is to keep the diastolic pressure below 105 mm Hg in order to prevent a brain hemorrhage or seizures in the mother.
Hypertension that develops before the 20th week of pregnancy is almost always due to pre-existing hypertension and not toxemia. High blood pressure that occurs only during pregnancy, called gestational hypertension, may start late in the pregnancy. These women do not have proteinuria, edema or convulsions and gestational hypertension appears to have no ill effects on the mother or fetus. This form of hypertension resolves shortly after delivery, although it may recur with subsequent pregnancies.
The use of medications for hypertension during pregnancy is controversial. The key question is, "At what level should the blood pressure be maintained?" The risk of untreated mild to moderate hypertension to the fetus or mother during pregnancy probably is not very large. Lowering the blood pressure too much can interfere with the flow of blood to the placenta and impair fetal growth. So, a compromise must be met. Not all mild or moderate hypertension during pregnancy needs to be treated with medication. If it is treated, the blood pressure should be reduced slowly and not to very low levels, not below 140/80.
Anti-hypertensive agents used during pregnancy need to be safe for normal fetal development. Beta-blockers, hydralazine (a vasodilator), labetalol (Normodyne, Trandate), alpha-methyldopa (Aldomet), and more recently, calcium channel blockers have been approved as suitable medications for hypertension during pregnancy. Some anti-hypertensive medications are not recommended (contraindicated) during pregnancy. These include ACE inhibitors, ARB drugs, and diuretics. ACE inhibitors may aggravate a diminished blood supply to the uterus (uterine ischemia) and cause kidney dysfunction in the fetus. ARB drugs may lead to death of the fetus. Diuretics can cause depletion of blood volume and impair placental blood flow and fetal growth.

Which medications are used to treat high blood pressure?
Angiotensin converting enzyme inhibitors (ACE Inhibitors) and angiotensin receptor blockers
The angiotensin converting enzyme (ACE) inhibitors and the angiotensin receptor blocker (ARB) drugs both affect the renin-angiotensin hormonal system which helps regulate blood pressure. ACE inhibitors by blocking (inhibiting) an enzyme that converts the inactive form of angiotensin in the blood to its active form. The active form of angiotensin constricts or narrows the arteries, but the inactive form cannot. With an ACE inhibitor as a single drug treatment (monotherapy), 50 to 60 percent of Caucasians usually achieve good blood pressure control. African American patients may also respond, but they require higher doses and frequently do best when an ACE inhibitor is combined with a diuretic. (Diuretics are discussed below.)
As an added benefit, ACE inhibitors may reduce an enlarged heart (left ventricular hypertrophy) in patients with hypertension. These drugs also appear to slow the deterioration of kidney function in patients with hypertension and protein in the urine (proteinuria). They have been particularly useful in slowing the progression of kidney dysfunction in hypertensive patients with kidney disease resulting from Type 1 diabetes (insulin-dependent). ACE inhibitors usually are the first line drugs to treat high blood pressure in cases that also involve congestive heart failure, chronic kidney failure in both diabetics and non-diabetics, and heart attack (myocardial infarction) that weakens the heart muscle (systolic dysfunction). ARB drugs are currently recommended for first line renal protection in diabetic nephropathy (kidney disease).
Patients treated with ACE inhibitors who also have kidney disease should be monitored for further deterioration in kidney function and high serum potassium. These drugs may be used to reduce the loss of potassium in people who are being treated with diuretics that cause patients to lose potassium. ACE inhibitors have few side effects. One bothersome side effect is a chronic cough. The ACE inhibitors include:
- enalapril (Vasotec),
- captopril (Capoten),
- lisinopril (Zestril and Prinivil),
- benazepril (Lotensin),
- quinapril (Accupril), perindopril (Aceon),
- ramipril (Altace),
- trandolapril (Mavik),
- fosinopril (Monopril), and
- moexipril (Univasc ).
For patients who develop a chronic cough on an ACE inhibitor, an ARB drug is a good substitute. ARB drugs work by blocking the angiotensin receptor (binder) on the arteries to which activated angiotensin must bind to have its effects. As a result, the angiotensin is not able to work on the artery. (Angiotensin is a hormone that constricts the arteries.) ARB drugs appear to have many of the same advantages as the ACE inhibitors but without the associated cough. They are also suitable as first line agents to treat hypertension.
ARB drugs include:
- losartan (Cozaar),
- irbesartan (Avapro),
- valsartan (Diovan),
- candesartan (Atacand),
- olmesartan (Benicar),
- telmisartan (Micardis), and
- eprosartan (Teveten).
In patients who have hypertension in addition to certain second diseases, a combination of an ACE inhibitor and an ARB drug may be effective in controlling the hypertension and also benefiting the second disease. This combination of drugs can treat hypertension and reduce the loss of protein in the urine (proteinuria) in certain kidney diseases and perhaps help strengthen the heart muscle in certain diseases of the heart muscle (cardiomyopathies). Both the ACE inhibitors and the ARB drugs are not to be used (contraindicated) in pregnant women. (See the section above on pregnancy.)
Beta-blockers
The sympathetic nervous system is a part of the nervous system that helps to regulate certain involuntary (autonomic) functions in the body such as the function of the heart and blood vessels. The nerves of the sympathetic nervous system extend throughout the body and exert their effects by releasing chemicals that travel to nearby cells in the body. The released chemicals bind to receptors (molecules) on the surface of the nearby cells and stimulate or inhibit the function of the cells. In the heart and blood vessels, the receptors for the sympathetic nervous system that are most important are the beta receptors. When stimulated, beta-receptors in the heart increase the heart rate and the strength of heart contractions (pumping action). Beta-blocking drugs acting on the heart slow the heart rate and reduce the force of the heart's contraction.
Stimulation of beta-receptors in the smooth muscle of the peripheral arteries and in the airways of the lung causes these muscles to relax. Beta-blockers cause contraction of the smooth muscle of the peripheral arteries and thereby decrease blood flow to body tissues. As a result, the patient may experience coolness in the hands and feet. In response to the beta-blockers, the airways are squeezed (constricted) by the contracting smooth muscle; this squeezing (impingement) on the airway causes wheezing, especially in individuals with a tendency for asthma. In short, beta-blockers reduce both the force of the heart's pumping action and the blood pressure that the heart generates in the arteries.
Beta-blockers remain useful medications in treating hypertension, especially in patients with a fast heartbeat while resting (tachycardia), cardiac chest pain (angina), or a recent heart attack (myocardial infarction). Beta-blockers appear to improve long-term survival when given to patients who have had a heart attack. Whether beta-blockers can prevent heart problems (are cardio-protective) in patients with hypertension any more than other anti-hypertensive medications is uncertain. Beta-blockers may be considered for treatment of hypertension because they also may treat co-existing medical problems; such as chronic anxiety or migraine headaches in people with hypertension. The common side effects of these drugs include depression, fatigue, nightmares, sexual impotence in males, and increased wheezing in people with asthma.
The beta-blockers include:
- atenolol (Tenormin),
- propranolol (Inderal),
- metoprolol (Toprol),
- nadolol (Corgard),
- betaxolol (Kerlone),
- acebutolol (Sectral),
- pindolol (Visken), and
- bisoprolol (Zebeta).
Diuretics
Diuretics are among the oldest known medications for treating hypertension. They work in the tiny tubes (tubules) of the kidneys to remove salt from the body. Water (fluid) also may be removed along with the salt. Diuretics may be used as single drug treatment (monotherapy) for hypertension. More frequently low doses of diuretics are used in combination with other anti-hypertensive medications to enhance the effect of the other medications.
The diuretic hydrochlorothiazide (Hydrodiuril) works in the far end (distal) part of the kidney tubules to increase the amount of salt that is removed from the body in the urine. In a low dose of 12.5 to 25 mg per day, this diuretic may improve the blood pressure - lowering effects of other anti-hypertensive drugs. The idea is to treat the hypertension without causing adverse effects sometimes seen with higher doses of hydrochlorothiazide. These side effects include potassium depletion and elevated levels of triglyceride (fat), uric acid, and glucose (sugar) in the blood.
Occasionally, when salt retention causing accumulation of water and swelling (edema) is a major problem, the more potent 'loop' diuretics may be used in combination with other anti-hypertensive medications. The loop diuretics are so called because they work in the loop segment of the kidney tubules to eliminate salt.
The most commonly used diuretics to treat hypertension include hydrochlorothiazide (Hydrodiuril), the loop diuretics furosemide (Lasix) and torsemide (Demadex), the combination of triamterene and hydrochlorothiazide (Dyazide), and metolazone (Zaroxolyn). For individuals who are allergic to sulfa drugs, ethacrynic acid, a loop diuretic, is a good option. Diuretics probably should not be used in pregnant women. (See the section above on pregnancy.)
Calcium channel blockers (CCBs)
Calcium channel blockers inhibit the movement of calcium into the muscle cells of the heart and arteries. Calcium is needed for these muscles to contract. Calcium channel blocker lower blood pressure by decreasing the force of the heart's pumping action (cardiac contraction) and relaxing the muscle cells in the walls of the arteries.
Three major types of calcium channel blockers are used. One type is the dihydropyridines, which do not slow the heart rate or cause other abnormal heart rates or rhythms (cardiac arrhythmias). These drugs include amlodipine (Norvasc), sustained release nifedipine (Procardia XL, Adalat CC), felodipine (Plendil), and nisoldipine (Sular).
The other two types of calcium channel blockers are referred to as the non-dihydropyridine agents. One type is verapamil (Calan, Covera, Isoptin, Verelan) and the other is diltiazem (Cardizem, Tiazac, Dilacor, and Diltia). Both the dihydropyridines and the non-dihydropyridines are very useful when used alone or in combination with other anti-hypertensive agents. The non-dihydropyridines are not recommended (contraindicated) in congestive heart failure. However, these same dihydropyridines are useful in preventing certain arrhythmias.
Many of the calcium channel blockers come in a short-acting form and a long-acting (sustained release) form. The short-acting forms of the calcium channel blockers may have adverse long-term consequences, such as strokes or heart attacks. These effects are due to the wide fluctuations in the blood pressure and heart rate that occur during treatment, resulting from the rapid onset and short duration of the short-acting compounds. When the calcium channel blockers are used in sustained release preparations less fluctuation occurs. The sustained release forms of calcium channel blockers are probably safer for long-term use. The main side effects of these drugs include constipation, swelling (edema), and a slow heart rate (only with the non-dihydropyridine types).
Alpha-blockers
Alpha-blockers lower blood pressure by blocking alpha-receptors in the smooth muscle of peripheral arteries throughout the tissues of the body. The alpha-receptors are part of the sympathetic nervous system, as are the beta-receptors. The alpha-receptors, however, serve to narrow (constrict) the peripheral arteries and the alpha-blockers cause the peripheral arteries to widen (dilate) and lower the blood pressure.
Recent evidence, suggests using alpha-blockers alone as a first line drug choice for hypertension may actually increase the risk of heart-related problems, such as heart attacks or strokes. Alpha-blockers, therefore, should not be used as an initial drug choice for the treatment of high blood pressure. Examples of alpha-blockers include terazosin (Hytrin) and doxazosin (Cardura).
Alpha-blockers are particularly useful in patients with enlargement of the prostate gland (which usually occurs in older men) because these drugs reduce the problems associated with urinating. The alpha-receptors, however, serve to narrow (constrict) the peripheral arteries and the alpha-blockers cause the peripheral arteries to widen (dilate) and lower the blood pressure. For example, tamsulosin (Flomax) or alfuzosin (Uroxatral) are alpha-blockers that work well in combination with other anti-hypertensive medications.
Clonidine
Clonidine (Catapres) is an antihypertensive drug that works centrally. That is, it works in a control center for the sympathetic nervous system in the brain. The drug is referred to as a central alpha agonist because it stimulates alpha-receptors in the brain. The result of this central stimulation is to decrease the sympathetic nervous system outflow and to decrease the stiffness (resistance) of the peripheral arteries. Clonidine lowers the blood pressure by relaxing (dilating or widening) the peripheral arteries throughout the body. This drug is useful as a second or third line drug choice for lowering blood pressure when other anti-hypertensive medications have failed. It also may be useful on an as-needed basis to control or smooth out fluctuations in the blood pressure. This drug tends to cause dryness of the mouth and fatigue so some patients do not tolerate it. Clonidine comes in an oral form or as a sustained release skin patch. For more information, please see the drug monograph on Clonidine.
Minoxidil
Minoxidil is the most potent of the drugs that lower blood pressure by dilating the peripheral arteries. This drug does not work through the peripheral sympathetic nervous system, as do the alpha and beta-blocker drugs, or through the control center in the brain, as does clonidine. Rather, it is a muscle relaxant that works directly on the smooth muscle of the peripheral arteries throughout the body. Minoxidil is used for patients who have not responded to any other medications. It must be combined with a beta-blocker or clonidine to prevent an increase in the heart rate and with a diuretic to prevent retention of fluid (swelling). Minoxidil may also increase hair growth.
What about the patient's compliance with medication regimes?
When uncomplicated hypertension has not caused symptoms, as often happens, some patients tend to forget about their medications. Patients also tend to fail to take their medications as prescribed (non-compliance or non-adherence) if they cause side effects. Quality of life issues are very important, especially with regard to compliance with prescribed blood pressure medications. Certain anti-hypertensive medications may cause such side effects as fatigue and sexual impotence which understandably can have profound effects on a patient's quality of life and compliance with treatment. More resistant cases of hypertension that require more medication may cause more adverse effects, and, therefore, less compliance.
In dosing schedules that require taking medication two to four times a day (split dose), some patients will remember to take their medicine only some of the times. In contrast, medications that can be given once daily tend to be remembered more regularly.
Expensive blood pressure medications, especially if insurance does not cover the costs, may also reduce compliance. People attempt to save money by skipping doses of the prescribed medication. The least expensive medication regimes use generic (not brand name) drugs, which are readily available for some of the diuretics and beta-blockers. Lifestyle changes such as losing weight, reducing dietary sodium, decreasing consumption of alcohol, and exercising regularly, the patient may require less medication.
Is alternative medicine used to treat high blood pressure?
Alternative medicine, also called integrative or complementary medicine, features the use of non-traditional (at least in the western world) techniques for treatment. For example, self-relaxation approaches to the therapy of hypertension include yoga, biofeedback, and meditation. These techniques can be effective in lowering the blood pressure, at least temporarily. In order to produce sustained reductions in the blood pressure these techniques may require hours of diligent adherence daily. They are generally practical only for few, highly motivated individuals with hypertension. Acupuncture has not yet been established as a standard or proven therapy for hypertension in the western world.
Certain herbal remedies have blood pressure-lowering components that may well be effective in treating hypertension. Most herbal remedies are available as food supplements, and the Food and Drug Administration (FDA) does not approve them as drugs. Therefore, herbal treatments for hypertension have not yet been adequately evaluated in scientifically controlled clinical trials for effectiveness and safety. In particular, their long-term side effects are unknown. A major problem with most herbal treatments is that their contents are not standardized. The ways in which herbal treatments work to lower blood pressure are not known and currently herbal remedies are usually not recommended for the treatment of hypertension.
What's new in high blood pressure?
A new class of anti-hypertensive drug, called a vasopeptidase blocker (inhibitor), has been developed. Uniquely, it works on two different systems at the same time. It blocks that part of the renin-angiotensin-aldosterone hormonal system that narrows (constricts) the peripheral arteries. It also blocks that part of the body's salt regulating system that conserves salt. Accordingly, this class of drug decreases the blood pressure by simultaneously dilating the peripheral arteries and increasing the body's loss of salt (natriuresis).
One such drug that is currently being studied is called omapatrilat. In laboratory animals with high blood pressure, this drug reduces the blood pressure and appears to protect the end-organs (heart, kidney, and brain) from damage by the high blood pressure. Moreover, the drug dilates the peripheral arteries, which increases blood flow to all tissues, and improves cardiac function in hypertensive patients with heart failure. Not yet approved by the FDA, omapatrilat is undergoing further testing to evaluate its effectiveness and safety.
sourceLast Editorial Review: 7/6/2007
|
Bookmark this post:
|
|


0 comments
Post a Comment